Estradiol acetate
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌɛstrəˈdaɪoʊl ˈæsəteɪt/ ES-trə-DY-ohl ASS-ə-tayt[1] |
| Trade names | Femtrace, Femring, Menoring |
| Other names | EA; E2A; E3A; Estradiol 3-acetate |
| Routes of administration | By mouth, vaginal (ring)[2] |
| Drug class | Estrogen; Estrogen ester |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.167.088 |
| Chemical and physical data | |
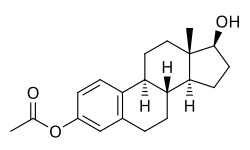
| Formula | C20H26O3 |
| Molar mass | 314.425 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Estradiol acetate (EA), sold under the brand names Femtrace, Femring, and Menoring, is an estrogen medication which is used in hormone therapy for the treatment of menopausal symptoms in women.[3][4][5][6] It is taken by mouth once daily or given as a vaginal ring once every three months.[2]
Side effects of estradiol acetate include breast tenderness, breast enlargement, nausea, headache, and fluid retention.[7][5][6] Estradiol acetate is an estrogen and hence is an agonist of the estrogen receptor, the biological target of estrogens like estradiol.[8][9] It is an estrogen ester and a prodrug of estradiol in the body.[9][8] Because of this, it is considered to be a natural and bioidentical form of estrogen.[9][10]
Estradiol acetate was introduced for medical use in 2001.[11] It is available in the United States and the United Kingdom.[11][3] The formulation for use by mouth has been discontinued in the United States.[12]
Medical uses
[edit]Estradiol acetate is used as a component of menopausal hormone therapy to treat and prevent menopausal symptoms such as hot flashes and osteoporosis in women.[13][14][15][16]
The Women's Health Initiative studies report increased health risks for menopausal women when using unopposed estrogens.[6] Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.[6]
Available forms
[edit]Estradiol acetate comes in the form of 0.45, 0.9, and 1.8 mg oral tablets (Femtrace) and in the form of 12.4 or 24.8 mg vaginal rings that release 50 or 100 μg/day estradiol for 3 months (Femring, Menoring).[5][6][17] However, the Femtrace product was discontinued in the United States.[12]
Contraindications
[edit]Contraindications of estrogens include coagulation problems, cardiovascular diseases, liver disease, and certain hormone-sensitive cancers such as breast cancer and endometrial cancer, among others.[18][19][20][21]
Side effects
[edit]The side effects of estradiol acetate are the same as those of estradiol. Examples of such side effects include breast tenderness and enlargement, nausea, bloating, edema, headache, and melasma.[7]
Overdose
[edit]Symptoms of estrogen overdosage may include nausea, vomiting, bloating, increased weight, water retention, breast tenderness, vaginal discharge, heavy legs, and leg cramps.[18] These side effects can be diminished by reducing the estrogen dosage.[18]
Interactions
[edit]Inhibitors and inducers of cytochrome P450 may influence the metabolism of estradiol and by extension circulating estradiol levels.[22]
Pharmacology
[edit]
Pharmacodynamics
[edit]Estradiol acetate is an estradiol ester, or a prodrug of estradiol.[9][8] As such, it is an estrogen, or an agonist of the estrogen receptors.[8][9] Estradiol acetate is of about 15% higher molecular weight than estradiol due to the presence of its C3 acetate ester.[3] Because estradiol acetate is a prodrug of estradiol, it is considered to be a natural and bioidentical form of estrogen.[9][10]
Pharmacokinetics
[edit]Estradiol acetate is converted into estradiol in the body.[9][8]
Chemistry
[edit]Estradiol acetate is a synthetic estrane steroid and the C3 acetate ester of estradiol.[3] It is also known as estradiol 3-acetate or as estra-1,3,5(10)-triene-3,17β-diol 3-acetate.[3] Another common ester of estradiol in use for oral administration is estradiol valerate, which is a C17β ester of estradiol.[8][23]
The experimental octanol/water partition coefficient (logP) of estradiol acetate is 4.2.[24]
| Estrogen | Structure | Ester(s) | Relative mol. weight |
Relative E2 contentb |
log Pc | ||||
|---|---|---|---|---|---|---|---|---|---|
| Position(s) | Moiet(ies) | Type | Lengtha | ||||||
| Estradiol | – | – | – | – | 1.00 | 1.00 | 4.0 | ||
| Estradiol acetate | C3 | Ethanoic acid | Straight-chain fatty acid | 2 | 1.15 | 0.87 | 4.2 | ||
| Estradiol benzoate | C3 | Benzoic acid | Aromatic fatty acid | – (~4–5) | 1.38 | 0.72 | 4.7 | ||
| Estradiol dipropionate | C3, C17β | Propanoic acid (×2) | Straight-chain fatty acid | 3 (×2) | 1.41 | 0.71 | 4.9 | ||
| Estradiol valerate | C17β | Pentanoic acid | Straight-chain fatty acid | 5 | 1.31 | 0.76 | 5.6–6.3 | ||
| Estradiol benzoate butyrate | C3, C17β | Benzoic acid, butyric acid | Mixed fatty acid | – (~6, 2) | 1.64 | 0.61 | 6.3 | ||
| Estradiol cypionate | C17β | Cyclopentylpropanoic acid | Cyclic fatty acid | – (~6) | 1.46 | 0.69 | 6.9 | ||
| Estradiol enanthate | C17β | Heptanoic acid | Straight-chain fatty acid | 7 | 1.41 | 0.71 | 6.7–7.3 | ||
| Estradiol dienanthate | C3, C17β | Heptanoic acid (×2) | Straight-chain fatty acid | 7 (×2) | 1.82 | 0.55 | 8.1–10.4 | ||
| Estradiol undecylate | C17β | Undecanoic acid | Straight-chain fatty acid | 11 | 1.62 | 0.62 | 9.2–9.8 | ||
| Estradiol stearate | C17β | Octadecanoic acid | Straight-chain fatty acid | 18 | 1.98 | 0.51 | 12.2–12.4 | ||
| Estradiol distearate | C3, C17β | Octadecanoic acid (×2) | Straight-chain fatty acid | 18 (×2) | 2.96 | 0.34 | 20.2 | ||
| Estradiol sulfate | C3 | Sulfuric acid | Water-soluble conjugate | – | 1.29 | 0.77 | 0.3–3.8 | ||
| Estradiol glucuronide | C17β | Glucuronic acid | Water-soluble conjugate | – | 1.65 | 0.61 | 2.1–2.7 | ||
| Estramustine phosphated | C3, C17β | Normustine, phosphoric acid | Water-soluble conjugate | – | 1.91 | 0.52 | 2.9–5.0 | ||
| Polyestradiol phosphatee | C3–C17β | Phosphoric acid | Water-soluble conjugate | – | 1.23f | 0.81f | 2.9g | ||
| Footnotes: a = Length of ester in carbon atoms for straight-chain fatty acids or approximate length of ester in carbon atoms for aromatic or cyclic fatty acids. b = Relative estradiol content by weight (i.e., relative estrogenic exposure). c = Experimental or predicted octanol/water partition coefficient (i.e., lipophilicity/hydrophobicity). Retrieved from PubChem, ChemSpider, and DrugBank. d = Also known as estradiol normustine phosphate. e = Polymer of estradiol phosphate (~13 repeat units). f = Relative molecular weight or estradiol content per repeat unit. g = log P of repeat unit (i.e., estradiol phosphate). Sources: See individual articles. | |||||||||
History
[edit]Estradiol acetate is relatively recent to the market, having been first approved in a vaginal ring formulation as Menoring in the United Kingdom in 2001,[13] followed by a vaginal ring formulation as Femring in the United States in 2002,[2] and finally as an oral preparation as Femtrace in the United States in 2004.[2][11]
Society and culture
[edit]Generic names
[edit]Estradiol acetate is the generic name of the drug and its USAN.[3]
Brand names
[edit]Estradiol acetate is marketed under the brand names Femtrace, Femring, and Menoring.[3][25][26]
Availability
[edit]Estradiol acetate is available in the United States and the United Kingdom.[11][3]
References
[edit]- ^ "Estradiol: Uses, Dosage & Side Effects". Drugs.com. Retrieved 21 April 2023.
- ^ a b c d Sivanandy MS, Masimasi N, Thacker HL (May 2007). "Newer hormonal therapies: lower doses; oral, transdermal, and vaginal formulations". Cleveland Clinic Journal of Medicine. 74 (5): 369–375. doi:10.3949/ccjm.74.5.369. PMID 17506242. S2CID 35423126.
- ^ a b c d e f g h "Estradiol Monograph for Professionals".
- ^ Buckler H, Al-Azzawi F (August 2003). "The effect of a novel vaginal ring delivering oestradiol acetate on climacteric symptoms in postmenopausal women". BJOG. 110 (8): 753–759. doi:10.1016/s1470-0328(03)02908-2. PMID 12892687.
- ^ a b c "Highlights of prescribing information" (PDF). accessdata.fda.gov. 2014. Retrieved 21 April 2023.
- ^ a b c d e "FEMRING". DailyMed. U.S. National Library of Medicine.
- ^ a b McIver B, Tebben PJ (23 September 2010). "Endocrinology". In Ghosh AK (ed.). Mayo Clinic Internal Medicine Board Review. OUP USA. pp. 222–. ISBN 978-0-19-975569-1.
- ^ a b c d e f Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ a b c d e f g Kuhnz W, Blode H, Zimmermann H (6 December 2012). "Pharmacokinetics of Exogenous Natural and Synthetic Estrogens and Antiestrogens". In Oettel M, Schillinger E (eds.). Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Handbook of Experimental Pharmacology. Vol. 135 / 2. Springer Science & Business Media. p. 261. doi:10.1007/978-3-642-60107-1_15. ISBN 978-3-642-60107-1.
Natural estrogens considered here include: [...] Esters of 17β-estradiol, such as estradiol valerate, estradiol benzoate and estradiol cypionate. Esterification aims at either better absorption after oral administration or a sustained release from the depot after intramuscular administration. During absorption, the esters are cleaved by endogenous esterases and the pharmacologically active 17β-estradiol is released; therefore, the esters are considered as natural estrogens.
- ^ a b Cirigliano M (June 2007). "Bioidentical hormone therapy: a review of the evidence". Journal of Women's Health. 16 (5): 600–631. doi:10.1089/jwh.2006.0311. PMID 17627398.
- ^ a b c d Ballagh SA (2004). "Vaginal rings for menopausal symptom relief". Drugs & Aging. 21 (12): 757–766. doi:10.2165/00002512-200421120-00001. PMID 15382956. S2CID 20717960.
- ^ a b "Drugs@FDA: FDA-Approved Drugs".
- ^ a b Speroff L (October 2003). "Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms". Obstetrics and Gynecology. 102 (4): 823–834. doi:10.1016/s0029-7844(03)00764-6. PMID 14551014. S2CID 10289535.
- ^ Al-Azzawi F, Lees B, Thompson J, Stevenson JC (2005). "Bone mineral density in postmenopausal women treated with a vaginal ring delivering systemic doses of estradiol acetate". Menopause. 12 (3): 331–339. doi:10.1097/01.gme.0000163870.03388.4d. PMID 15879923. S2CID 22295565.
- ^ Utian WH, Speroff L, Ellman H, Dart C (2005). "Comparative controlled trial of a novel oral estrogen therapy, estradiol acetate, for relief of menopause symptoms". Menopause. 12 (6): 708–715. doi:10.1097/01.gme.0000184220.63459.a8. PMID 16278614. S2CID 28927438.
- ^ Speroff L, Haney AF, Gilbert RD, Ellman H (2006). "Efficacy of a new, oral estradiol acetate formulation for relief of menopause symptoms". Menopause. 13 (3): 442–450. doi:10.1097/01.gme.0000182802.06762.b2. PMID 16735941. S2CID 19563197.
- ^ Lowdermilk DL, Perry SE, Cashion MC, Alden KR (18 December 2014). "Reproductive System Concerns". Maternity and Women's Health Care - E-Book. Elsevier Health Sciences. pp. 137–. ISBN 978-0-323-39019-4.
- ^ a b c Lauritzen C (September 1990). "Clinical use of oestrogens and progestogens". Maturitas. 12 (3): 199–214. doi:10.1016/0378-5122(90)90004-P. PMID 2215269.
- ^ Lauritzen C, Studd JW (22 June 2005). Current Management of the Menopause. CRC Press. pp. 95–98, 488. ISBN 978-0-203-48612-2.
- ^ Laurtizen C (2001). "Hormone Substitution Before, During and After Menopause" (PDF). In Fisch FH (ed.). Menopause – Andropause: Hormone Replacement Therapy Through the Ages. Krause & Pachernegg: Gablitz. pp. 67–88. ISBN 978-3-901299-34-6.
- ^ Midwinter A (1976). "Contraindications to estrogen therapy and management of the menopausal syndrome in these cases". In Campbell S (ed.). The Management of the Menopause & Post-Menopausal Years: The Proceedings of the International Symposium held in London 24–26 November 1975 Arranged by the Institute of Obstetrics and Gynaecology, The University of London. MTP Press Limited. pp. 377–382. doi:10.1007/978-94-011-6165-7_33. ISBN 978-94-011-6167-1.
- ^ Cheng ZN, Shu Y, Liu ZQ, Wang LS, Ou-Yang DS, Zhou HH (February 2001). "Role of cytochrome P450 in estradiol metabolism in vitro". Acta Pharmacologica Sinica. 22 (2): 148–154. PMID 11741520.
- ^ Düsterberg B, Nishino Y (December 1982). "Pharmacokinetic and pharmacological features of oestradiol valerate". Maturitas. 4 (4): 315–324. doi:10.1016/0378-5122(82)90064-0. PMID 7169965.
- ^ "Estradiol acetate | C20H26O3 | ChemSpider". www.chemspider.com. Retrieved 21 April 2023.
- ^ U.S. Food and Drug Administration (2009). Menopause - Medicines to Help You. GPO FCIC. pp. 3–. ISBN 978-1-61221-026-1.
- ^ Fritz MA, Speroff L (28 March 2012). "Postmenopausal Hormone Therapy". Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. pp. 757–. ISBN 978-1-4511-4847-3.















