Wikipedia talk:WikiProject Pharmacology
| This is the talk page for discussing WikiProject Pharmacology and anything related to its purposes and tasks. |
|
| Archives: Index, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17Auto-archiving period: 3 months |
| This project page does not require a rating on Wikipedia's content assessment scale. It is of interest to the following WikiProjects: | ||||||||
| ||||||||
| WikiProject Pharmacology was featured in a WikiProject Report in the Signpost on 17 January 2009. |
|
|
This page has archives. Sections older than 90 days may be automatically archived by Lowercase sigmabot III when more than 10 sections are present. |
Finding "undocumented" compounds
[edit]Hi, I'm not sure if this is the right place to ask this.
I've seen a lot of pharmacology navboxes (such as muscarinic receptor modulators, for an example), lots of them contain a lot of drugs that are not really known (a lot of them are redlinks), which is what I mean by "undocumented compounds"
I was just curious if anyone knew how to find names of these compounds (like specific keywords in a search engine)
Because so far I've been creating a lot of articles that were redlinks on the navboxes, but I'd love to add new compounds to said templates.
So if anyone knew how to find lists (or something similar) with names of investigational drugs (names like "ADX-71441") that would be really great Themonkey942 (talk) 22:29, 7 September 2024 (UTC)
Importance ratings need review
[edit]An editor first labeled Legality of cannabis as top-importance for this group, and after I removed the rating, has changed it to high-importance. Please decide for yourselves how you'd like to have it assessed.
I've seen a couple of editors "upgrade" their favorite subjects, perhaps in the mistaken belief that this will result in more editors working on the articles. I specifically suggest taking a look at what's in Category:Top-importance pharmacology articles and Category:High-importance pharmacology articles in particular, to see whether any spammers have been at work. WhatamIdoing (talk) 04:41, 26 September 2024 (UTC)
Dose and dosage
[edit]Is there a good, well-sourced page that describes the technical difference between dose and dosage? WhatamIdoing (talk) 17:52, 30 September 2024 (UTC)
- Apparently we did not have such an article, but I created dosage (pharmacology) which hopefully is a start. Boghog (talk) 18:58, 30 September 2024 (UTC)
- Thanks for creating that. WhatamIdoing (talk) 19:41, 30 September 2024 (UTC)
- Perhaps dosage (pharmacology) should be merged into Medical prescription. Thoughts? Boghog (talk) 19:48, 30 September 2024 (UTC)
- I'm inclined not to make a hasty decision (either way). Part of this is because I generally prefer merging, but other people tell me that a short, focused article is better for mobile users (which is most of our page views).
- I did some copyediting on Dose (biochemistry). WhatamIdoing (talk) 20:27, 30 September 2024 (UTC)
- In my opinion, a dosage and a prescription are two different (albeit related, of course) things. I'd be inclined not to merge, for that reason. --Tryptofish (talk) 20:44, 30 September 2024 (UTC)
- Perhaps dosage (pharmacology) should be merged into Medical prescription. Thoughts? Boghog (talk) 19:48, 30 September 2024 (UTC)
- Thanks for creating that. WhatamIdoing (talk) 19:41, 30 September 2024 (UTC)
- My view is that they are synonyms, and, with respect ot Boghog for work done, I don't think that we need that new page. Indeed, my reading of the key source in that new article is not consistent with the definition in the lede. Rowbotham et al (2019) actually say
we found dose and dosage to be used interchangeably. We recommend a distinction between these terms, with ‘dosage’ having the advantage of capturing change to amount ‘dispensed’ over time (in response to effects achieved). Dosage therefore acknowledges the inevitable dynamic and complexity of implementation
. So, the current state is that they are synonyms; their recommended use is a very subtle one that doesn't reflect the lede of the current article. My own UK-centric view is that dosage is an abomination that should be eliminated wherever it rears its ugly head, and that the term dose suffices for all civilized discussion. Given that bias, I suggest merging Dosage (pharmacology) to Dose (biochemistry), describing any differences in use on that page. Klbrain (talk) 21:56, 2 October 2024 (UTC)- Dorland's (2007) gives these definitions:
- dosage
- the determination and regulation of the size, frequency, and number of doses.
- dose
- quantity to be administered at one time, such as a specified amount of medication.
- The latter continues for three-quarters of a page to cover all the sub-definitions (e.g., total dose, daily dose, median effective dose...), but they don't use them as synonyms. That said, even though there is a verifiable technical distinction between the two, I think we could still merge the articles. It is not unusual for an article to have a note about the technical distinction between two words, especially when that distinction is more often ignored outside of technical documents. And to go even further than Klbrain, we might want to consider using the plain old English word amount when appropriate, for even greater clarity. WhatamIdoing (talk) 22:44, 2 October 2024 (UTC)
- See also Collins: dosage and Collins: dose. My understanding of the two terms matches what has been written in the Wikipedia articles. I suggest changing "given at one time" to "given at any one time" in case anyone thinks dose only refers to a one-off consumption. And that definition seems to match what Collins says is the British English use, as far as medicine is concerned. However, the US English use (citing Websters and their own definition in two sections) suggests some ambiguity with "the amount used in a dose" and "the amount of medicine to be given". At first this seems to indicate Americans are sometimes using "dosage" where they should say "dose" but then I considered what "amount" means, and it is cumulative.
- WAID mentions both "total dose" and "daily dose" which are different from an individual dose. A medicine of 100mg taken three times a day for two days has an individual dose of 100mg, daily dose of 300mg and total dose of 600mg. In each case the word dose is used, not dosage, though we might qualify use of the word that isn't referring to the individual dose if that isn't clear. Sometimes the word on its own can refer to the quantity consumed daily or in total. For example, if someone suffered ill effects from being on "too high a dose" of a medicine, this could be because they are taking it four times a day rather than two. If someone died from being given a "huge dose" of a medicine, this could be because the dose consumed over three days was ultimately fatal, whereas one individual dose might not. This all says to me that dose can be used to refer to an accumulation. The worse "dosage" couldn't be used for that at all.
- So perhaps in addition to "at any one time" (the individual dose) we could say "or in total over a period" (the daily dose or total dose). The American English usages in Collins would permit that definition. Have we got a source that say so more explicitly? -- Colin°Talk 08:00, 3 October 2024 (UTC)
- I see that in Dose (biochemistry)#Vaccines it says "Vaccinations are typically administered as liquids and dosed in milliliters" Clearly this isn't millilitres of vaccine. For example this Covid vaccine is a 0.3ml dose containing 30 micrograms of the vaccine. A liquid medicine such as Epilim liquid is 200mg/5ml. The dose in that case might refer to 400mg twice a day or 10ml twice a day or most precisely as 400mg as 10ml twice a day. One doesn't care about the size of a pill, though one might need to take two pills if the dose requires it.
- As the lead of of Dose (biochemistry) says, it can refer to the taking of some unit of medicine without anyone giving a size in mg or ml. For example this government report says "Up to 23 August 2022, 53 million people received a first dose of COVID-19 vaccine, 50 million received a second dose and 40 million received a third or booster dose."
- I wonder if the dose article could say more about how sometimes dose references the quantity of the containing liquid or pills rather than the amount of medicinal compound. "Take two paracetamol". "Draw up 0.3ml of covid vaccine from the vial". "Take 30ml of cough medicine". -- Colin°Talk 08:30, 3 October 2024 (UTC)
- I think that Dose (biochemistry), though not even close to our worst articles, is sufficiently weak that any editor who's looked in a dictionary/has a basic grasp of the concept could improve it through a quick copyedit. WhatamIdoing (talk) 19:54, 3 October 2024 (UTC)
- Dorland's (2007) gives these definitions:
- Look the drug up by full name in most wifi and ull find all that sort of info : 2600:1000:A121:5319:712C:16E4:EA57:57EE (talk) 22:27, 13 November 2024 (UTC)
Good article reassessment for Mephedrone
[edit]Mephedrone has been nominated for a good article reassessment. If you are interested in the discussion, please participate by adding your comments to the reassessment page. If concerns are not addressed during the review period, the good article status may be removed from the article. Z1720 (talk) 16:10, 12 October 2024 (UTC)
External links in list articles
[edit]I noticed the new list of investigational autism and pervasive developmental disorder drugs today, which is one of many articles submitted via AfC by the prolific IP editor 76.174.0.57. The list is clearly worthwhile but I do note that it has 89 external links in its main sections and only three actual references. This seems to go against the guidance at WP:ELLIST but is common in similar lists of interest to the Pharmacology Project. Some of the external links may be totally unnecessary, since there are valid wikilinks to existing articles where reference sources can be found. In other cases, it might be better to convert the EL to cites. Is this worth discussion and agreement on a consistent approach? Mike Turnbull (talk) 14:53, 28 October 2024 (UTC)
- Fine for the links to be turned into refs. It's mostly just that it's too overwhelming to do it myself. Especially considering that the lists require regular updating, which usually entails remaking them from scratch. Ideally turning the refs into links would be automated via a batch method somehow. But I'm not aware of a tool for that. (Perhaps User:Boghog might, since I see them templating a lot of bare URLs?) I will admit that it is also significantly easier to check the status of the drugs (e.g., many at once) when the cites are formatted as external links rather than as refs though. But if Wikipedia policy dictates that they should be formatted as refs then that's how they should be. – 76.174.0.57 (talk) 21:45, 28 October 2024 (UTC)
- I went ahead and converted the external links into citation tags. Although this might make them slightly harder to follow, templated citations could be useful when turning the red drug links into stubs. For anyone interested, pasting the following RegEx into the "search and replace" function of Wikipedia’s editing toolbar will convert the external links into refs containing bare URLs:
Search for: \[https(.*?)\]
Replace with: <ref>https\1</ref>
- In a second step, the WP:reFill (link) tool will convert the bare URLs into {{cite web}} templates. Boghog (talk) 06:51, 29 October 2024 (UTC)
- @Boghog Thanks for teaching me something new and useful! I'm going to apply that technique to the other lists I linked above. Two comments: 1) the search string needs to be
\[http(.*?)\]in older articles using http rather than https and 2) you had a typo in your replace string, which should be<ref>https$1</ref>Had me fooled for a moment! Mike Turnbull (talk) 13:24, 29 October 2024 (UTC)- @Mike Turnbul I forgot about non-secure URLs. Good catch. Alternatively, the search regex could be modified to
\[https?(.*?)\]. "s?" will match zero or one occurrence of "s", and hence will match both "http" and "https". The back reference designation for most regex parsers I am familiar with is "\1" which worked when I tested it. When I tried "$1", instead of inserting the captured URL, it inserted literally "$1". So I am a bit confused by your second statement. Boghog (talk) 13:59, 29 October 2024 (UTC)- @Boghog I've had little experience with regex searches but when I tried your original "\1" version this was the diff, which I reverted as it had added the "\" into the output. I then looked at the table in Regular_expression#Examples, where the second row on bracketed groups says that $1 can be used "later" to refer to the matched pattern. I then used the $ version successfully. My instinct is always to do the experiment and when something works I rarely worry about why it did! That entry in the table does say that some implementations use "\1". Mike Turnbull (talk) 14:41, 29 October 2024 (UTC)
- @Mike Turnbul I forgot about non-secure URLs. Good catch. Alternatively, the search regex could be modified to
- @Boghog Thanks for teaching me something new and useful! I'm going to apply that technique to the other lists I linked above. Two comments: 1) the search string needs to be
- Such a simple solution. Thanks Boghog and Mike Turnbull. Saved an otherwise huge amount of work. – 76.174.0.57 (talk) 21:08, 29 October 2024 (UTC)
Contra TAAR1 agonism as the mediator of amphetamine actions
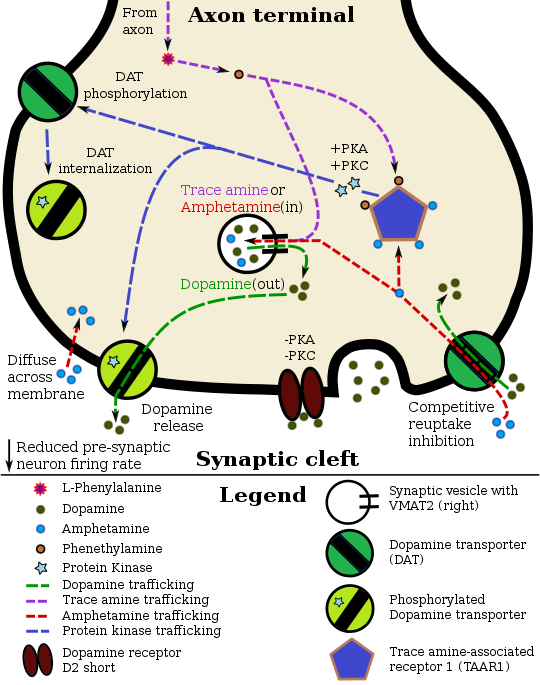
[edit]It is widely stated or implied across the English Wikipedia that amphetamine and related monoamine releasing agents (MRAs) induce their effects by agonism of the trace amine-associated receptor 1 (TAAR1). This notion is generally presented as fact and is stated in many relevant Wikipedia articles (e.g., amphetamine, methamphetamine, dextroamphetamine, Adderall, lisdexamfetamine, MDMA, stimulant, trace amine, TAAR1, etc.). It is even presented in figures (e.g., Template:Amphetamine pharmacodynamics).
The promotion of this theory seems to have originated with User:Seppi333, who has done a large amount of seemingly excellent work on the amphetamine and related articles. User:Seppi333 cites studies published in the 2000s by Xie and Miller and colleagues who found that monoamine transporter (MAT) reversal and monoamine efflux induced by phenethylamine and amphetamines (edit: methamphetamine) was dependent on TAAR1 activation in-vitro.[1][2][3][4] These findings would appear to substantiate the theory.
While I respect and appreciate User:Seppi333 and his hard work on the amphetamine-related content on Wikipedia, I have strong reservations about the TAAR1 activation theory and the widespread promotion of this theory on Wikipedia. The reasons for this are numerous, and include the following:
- TAAR1 is non-essential for amphetamine actions in vitro and in vivo: Amphetamines and other MRAs continue to induce monoamine efflux and other MRA-type actions like DAT internalization in vitro in human embryonic kidney 293 (HEK293) cells transfected with MATs.[5][6][7][8][9][10][11][12] This is notable as these non-neuronal cells do not express the TAAR1.[5] Likewise, amphetamines continue to increase monoamine release and produce stimulant-type behavioral effects in vivo in TAAR1 knockout mice (more on that below).[13][14][15]
- Many MRAs do not activate TAAR1 or do so very weakly: There are many MRAs that do not activate the human TAAR1 (EC50 > 30 μM). These include methcathinone, mephedrone, flephedrone, brephedrone, ephedrine, 4-methylamphetamine, PMA, 4-MTA, MDEA, MBDB, 5-APDB, 5-MAPDB, mCPP, TFMPP, and methylhexanamine (DMAA), among others.[16][5] Hence, TAAR1 agonism again appears to be non-essential for induction of monoamine release by MRAs. In addition, many amphetamines that do act as TAAR1 agonists, including amphetamine, methamphetamine, and MDMA, only activate the human TAAR1 at micromolar concentrations that are far higher than their nanomolar potencies for inducing monoamine release in vitro, and hence may not be pharmacologically relevant in humans.[16][17] Also, in contrast to many other MRAs acting as TAAR1 agonists, MDA and MDMA are notable in actually being weak partial agonists of the human TAAR1 (Emax ≈ 11–26%). As such, they seem more likely to be antagonist-like than agonist-like at the TAAR1.[16][18]
- TAAR1 signaling is antidopaminergic and anti-reinforcing: TAAR1 activation robustly inhibits the striatal dopaminergic and rewarding effects of amphetamines and of other reinforcing drugs like cocaine, opioids, and alcohol.[3][19][20][21][22][23][24] This has been shown with TAAR1 agonists[25][26] and with TAAR1 overexpression.[27] Moreover, TAAR1 knockout mice are supersensitive to the monoamine release and behavioral effects of stimulants and MDMA.[13][15][14][28] Accordingly, TAAR1 agonists like ulotaront do not have amphetamine-like effects in animals and show no misuse potential.[29] In addition, TAAR1 agonism produces robust aversive effects in animals.[30][31] Relatedly, it has been proposed that TAAR1 agonism by amphetamines serves to auto-inhibit and constrain their effects.[14] It has also been suggested by some researchers that lack of TAAR1 agonism with cathinones like mephedrone may enhance their reinforcing effects relative to amphetamines.[32] Due to their antidopaminergic and hence antipsychotic-like effects, TAAR1 agonists like ulotaront are being studied for treatment of schizophrenia and have reached late-stage clinical trials for this indication.[33][34] Similarly, TAAR1 agonists are being investigated for potential antagonistic therapy of psychostimulant addiction.[35][20][24]
- Experts on MRAs do not implicate TAAR1 signaling: Major literature reviews by top experts on MRAs, such as Richard B. Rothman and David J. Heal, state that the mechanism by which amphetamines induce monoamine release is unknown or poorly understood, and do not implicate TAAR1 activation.[36][37][38][39] Rothman and his group are notable in being prominent NIDA researchers and in having developed the major in-vitro assay that is used to evaluate the releasing actions of MRAs.[40] In my experience, it has been hard to find secondary source literature in general that presents TAAR1 activation as mediating amphetamine or MRA actions. It would seem to be an obscure idea in the literature.
- An expert critiques Wikipedia's TAAR1 MRA theory: Matthew Baggott, a major MDMA researcher, founder of Tactogen (a company developing novel MDMA-like MRAs as medicines), and collaborator with the Rothman/NIDA group, has criticized and discounted Wikipedia's TAAR1 theory of MRA action on social media.[41][18][42][17][43] He has provided various arguments against it in his posts, including several of the above points. The following quote gives an idea: "My take is that TAAR1 agonism is misunderstood, especially on Wikipedia, and it decreases the effects of stimulants. TAAR1 knockout mice have increased effects of stimulants (eg here) while mice that overexpress TAAR1 have less sensitivity (eg here). A TAAR1 agonist is potentially a novel way to decrease dopamine activity."[41]
I should note that TAAR1 agonism paired with concomitant uptake by MATs (i.e., MAT substrate activity) is a key part of the TAAR1 MRA theory and might help to explain differences between non-MRA TAAR1 agonists and amphetamine-type MRAs acting as TAAR1 agonists.[4] (The TAAR1 is an intracellular receptor, and uptake by MATs would in theory result in more potent activation of TAAR1 in the subset of neurons that co-express TAAR1 and MATs.) However, this still does not seem to account for many of the other findings that contradict the theory described above.
I have had reservations and suspicions about the TAAR1 and MRAs theory here on Wikipedia for years. However, I'm not an expert in this subject area and I thought I might be missing something. As a result, I opted not to raise my concerns. In any case, coming across Matthew Baggott's critiques of the theory on social media finally changed my mind and motivated me to act.
User:Seppi333 and any others, if there is something I'm missing, I'm open to being enlightened. But, considering all of the above, I don't think I'm wrong here. It appears to me that TAAR1 agonism may modulate the effects of MRAs, and theoretically might play some role in monoamine release induction in the case of some MRAs (per those Xie/Miller et al. in-vitro studies). However, it seems that the available research is overall strongly in conflict with the idea that TAAR1 activation is responsible or essential for monoamine release induced by amphetamine or MRAs generally.
Based on the above, I propose that a major clean up of the relevant content on Wikipedia may be in order.
Also pinging User:Professional Crastination, since they have done some editing on the relevant pages as well and may have input.
Thank you. – AlyInWikiWonderland (talk, contribs) 10:45, 13 December 2024 (UTC)
- Wikipedia doesn’t suggest TAAR1 is a mediator of the mode of action of MRAs, but hey if you want to dispute the fact that it’s not central to amphetamine’s pharmacology, I’ll make you and “Matthew Baggott” look like retards. Never call me out like this again. Seppi333 (Insert 2¢) 22:02, 13 December 2024 (UTC)
- Reminder: WP:CIV and WP:NPA. I didn't mean to infringe on your ego. This is about the content and its factual accuracy. And about whether said content reflects scientific consensus. I care about those things. And to me, something seems very off in this area. Please try to see it from others' perspectives.
- You state this:
Wikipedia doesn’t suggest TAAR1 is a mediator of the mode of action of MRAs, [...]
But the amphetamine, dextroamphetamine, methamphetamine, and many other relevant articles appear to implicate TAAR1 in mediating amphetamine-/MRA-induced monoamine reuptake inhibition and release (MAT internalization, reverse transport, and/or efflux). Many of these articles seem to present TAAR1 agonism as the foremost and key action of amphetamines, even before their well-accepted status as MRAs. Per everything I wrote above, there appear to be many strong points that go against TAAR1 mediation of amphetamine and MRA actions. Moreover, TAAR1 mediating the monoamine release induced by amphetamine and other MRAs does not appear to be widely accepted or scientific consensus, yet Wikipedia is currently presenting it like it is. As indicated by social media, many laypersons have the impression that TAAR1 mediates the MRA actions of amphetamines, and that appears to be because of Wikipedia. As far as I'm aware, you are responsible for most of the relevant Wikipedia content in this area. Something seems very wrong here to me, and apparently to others like Baggott (an expert on MRAs). The burden is on you to substantiate and explain this.
- You state this:
- I asked you about this topic years ago in private and IIRC you linked me to one of the Xie and Miller papers. While those studies do provide basic in-vitro mechanistic substantiation, those studies, in light of all of the contradicting findings, haven't been satisfactory for me on their own and I've continued to feel conflicted and confused. If I'm somehow mistaken about things, please explain them to me. As I mentioned, I would be happy to be enlightened. But it is very difficult for me to see how all of the counterpoints can be reconciled with what's currently presented on Wikipedia. Thus my raising of these concerns publicly and interest in refactoring the relevant content.
- Lastly, I'm not specifically contesting that TAAR1 agonism may be involved in and modulatory of amphetamine effects. I'm challenging the notion that TAAR1 agonism is key for amphetamine-/MRA-induced monoamine release (as well as MRA-type reuptake inhibition). And, by extension, for their consequent effects like psychostimulant or entactogen effects. (However, considering the micromolar EC50 values of amphetamine and other related MRAs for hTAAR1[16] and Baggott's comments in this area,[17][42][41] I do have some suspicions about whether TAAR1 agonism is indeed a significant action of amphetamine in humans at all as well. Is there any in-vivo primate or human evidence that demonstrates definitive involvement of TAAR1 agonism in amphetamine effects? Because if not, then I would relegate that idea to the status of an open question rather than proven fact also.) – AlyInWikiWonderland (talk, contribs) 04:45, 14 December 2024 (UTC)
- Sigh. If you actually read the articles, you'd realize its the drug's action at TAAR1 and VMAT2 TOGETHER that mediate its mechanism of action as an MRA. It is NOT TAAR1 alone, which is basically what every paper i've cited which mentions amphetamine and also states that TAAR1 agonists are anti-addictive says.
- I don't have any burden of proof to worry about. Nice attempt, though. Why? Amphetamine is an FA and if you try making bullshit changes like what you're implying, you'll be reverted by other people who are actually active on WP. I seriously think you're just trolling me, but if you're actually genuinely concerned, you need to read the papers a lot more closely. Seppi333 (Insert 2¢) 07:57, 14 December 2024 (UTC)
- For what it's worth, I apologize for coming off so angrily. Bad day. Edit: Sorry for being an asshole. I'll follow up more tomorrow. It seems like you are being genuine. Seppi333 (Insert 2¢) 08:18, 14 December 2024 (UTC)
- Alright. So per your account, it's TAAR1 and VMAT2 together (in addition to plasmalemmal MAT uptake/substrate activity) that allow for mediation of MRA actions. Aside from further adding to why MRAs acting as TAAR1 agonists and non-MRA TAAR1 agonists are different however, I don't see how this changes things re: the other points I raised (but what User:Professional Crastination said partly does; more on that below). Moreover, several notable MRAs, including phenmetrazine, phentermine, and benzylpiperazine, are inactive at VMAT2 per the Rothman group.[36][44] Others like mephedrone also show only weak VMAT2 activity.[45] Phenmetrazine is notably a robust NDRA with similar effects to amphetamine and methamphetamine. So VMAT2 activity would appear to be non-essential for marked monoamine release with MRAs. To me, this would seem to add another point against the theory. How would you explain that?
- I am indeed being genuine. Another reminder: WP:AGF. In any case, thank you for dialing things down. – AlyInWikiWonderland (talk, contribs) 00:27, 16 December 2024 (UTC)
- There are so many other possible mechanisms you are discounting simply to "disprove" how amphetamine works. Maybe they strongly upregulate DA synthesis prior to vesicular uptake. Perhaps they inhibit DA breakdown within the cytosol of DA neurons. Have all those and other theories been tested? Again, the only thing I really know is how AMPHETAMINE works, not MRAs in general. And there are so many possible mechanisms of action that would explain an increased cytosolic load of dopamine besides VMAT2 inhibition. Seppi333 (Insert 2¢) 10:28, 16 December 2024 (UTC)
- I am pointing out inconsistencies in your personal theory of how amphetamine works. Your suggestions for how to resolve this particular inconsistency involve additional assumptions and mechanisms for numerous MRAs. The weak VMAT2 activity of mephedrone notably also appears to extend to other cathinones, such as methcathinone and methylone.[46][47] A more parsimonious account is that VMAT2 inhibition/reversal and increased cytosol monoamine levels are not actually required for efficacious monoamine release with MRAs generally. Indeed, amphetamine can still release dopamine without VMAT2.[48] In fact, it appears that VMAT2 involvement in the actions of amphetamines is actually controversial and uncertain.[48][49][46]
- Interestingly, there is also a whole alternative model of amphetamine action involving promotion of exocytotic dopamine release and enhancement of phasic dopamine signaling based on in-vivo animal findings.[50][48][51] Per these researchers, this might actually be how amphetamine works at "low" doses (like those used therapeutically), and augmentation of DAT efflux and tonic dopaminergic signaling may be more relevant to high misused and/or toxic doses.[50][48][51] (The quite comprehensive Reith & Gnegy (2020) review notably covers this theory, yet, again, does not even mention your TAAR1 agonism theory.[48])
- If VMAT2 activity is also non-essential for induction of monoamine release and robust associated effects, then I feel that that seriously further calls into question your model involving TAAR1 agonism. I hope the preceding also further emphasizes how much uncertainty and disagreement there remains in the scientific community in general about how amphetamine and other MRAs act. I think you are being overconfident in your particular view and aren't giving other views proper consideration (both personally and in terms of Wikipedia content). The truth is that we don't have full understanding nor scientific consensus on how amphetamines work and different theories and postulated mechanisms are still being evaluated.
- I'll respond to the other comments here later, have to go for now. – AlyInWikiWonderland (talk, contribs)
- Hey everyone. I was pinged here so I'm going to post my input. I'm not sure where exactly I should place my first reply as discussion is already under way, but I'll place it under @Seppi333's most recent reply because I think this will serve as an extension of it, if only because I believe he will benefit from some R&R in response to whatever happened off-wiki today and in the meantime it will give @AlyInWikiWonderland something to consider Re:
TAAR1 and amphetamine
. - Before I continue, I'd like to apologise in advance for the late reply. I was at The Killers last night and then went to the zoo with my partner today. Secondly, I'm also apologising in advance for any awkwardly worded sentences I may have written in this reply; I haven't had the privilege of the best quality sleep over the last few nights, and even though I take a medication that is sometimes used to treat excessive daytime sleepiness, I'm still very capable of making fatigue-related task errors that seem unfathomable in real time :P. Don't worry though, I love my ~8-9 hours of sleep a night as much as the next person.
- Lastly, I should also point out that much of my edits on the amphetamine and methamphetamine articles have been concentrated on the uses/medical section. Seppi wrote much, if not all of the pharmacology section, so I imagine they would be the best person to clarify any concerns you have about the coverage of TAAR1 by doing what they do best a la supplying a technically nuanced essay on the subject.
- The idea that TAAR1’s involvement is overstated in the coverage of pharmacology on the amphetamine wikipedia article isn't reflective of the available evidence. TAAR1 is unequivocally a major intracellular target of amphetamine, but it does not act in isolation. Amphetamine-induced monoamine efflux is mediated through multiple signalling cascades that regulate DAT function, including pathways that happen to be initiated by TAAR1 activation and protein kinase activity downstream, as well as of other possible unidentified targets in monoamine neurons (e.g., CAMKII).
- For context, TAAR1 activation triggers PKA- and PKC-dependent phosphorylation of DAT, which facilitates reverse transport/MA efflux and transporter internalisation respectively (NB: whether DAT is internalised or reversed is dependent on the residues phosphorylated). RhoA activation, which leads to ROCK-dependent internalisation of DAT and EAAT3, occurs downstream of TAAR1. This RhoA-driven process is transient because PKA inactivates RhoA after a short period, at which point PKA-mediated DAT internalisation dominates. Importantly, these cascades do not occur spontaneously. Amphetamine induces efflux through DAT via signalling cascades that involve kinase-dependent transporter phosphorylation. Amphetamine's entrance into the plasma membrane — whether by DAT uptake or passive diffusion — does not directly cause transporter phosphorylation. Rather, it signals through intracellular biomolecular targets, such as TAAR1 or others that are yet-to-be identified, to activate protein kinases that phosphorylate DAT via that signalling cascade. Amphetamine itself does not donate a phosphate group to the protein.
- Also, to expand on what Seppi stated Re:
" its the drug's action at TAAR1 and VMAT2 TOGETHER that mediate its mechanism of action as an MRA"
: cytosolic DA that's derived from amphetamine's action at VMAT2 significantly amplifies the magnitude of DA involved in DAT-mediated efflux, but without intracellular signalling through a kinase (e.g., TAAR1 --> PKC or unidentified target ----> CAMKII-alpha), there is no known mechanism that links VMAT2-driven DA release to DAT phosphorylation. If amphetamine had no effect on VMAT2, DAT would still be phosphorylated, and DA efflux would occur, but the magnitude would naturally be mardkedly reduced relative to the scenario where amphetamine interacts with VMAT2 and causes the collapse of the vesicular pH gradiant as a consequence. - Below is a table written put together by Seppi333 that encomapsses much of the research on amphetamine and its (known) kinase-mediated signalling cascades based on the avaliable evidence as of 2019. This table is supposed to support an updated model of the amphetamine pharmacodynamics table, but that's yet to come. As an aside, I was actually going to take a crack at updating the SVG for that template a few weeks ago, as my more notable edits in 2024 have been concerned with significantly expanding coverage of amphetamine and its transcluded articles so that they're up-to-date (e.g., adding content on the efficacy of its non-ADHD medical indications narcolepsy and binge eating disorder). However, in consistency with my relevant-as-ever username, I placed that at the back of my to-do pile if only because graphic design is not my passion.
- Hey everyone. I was pinged here so I'm going to post my input. I'm not sure where exactly I should place my first reply as discussion is already under way, but I'll place it under @Seppi333's most recent reply because I think this will serve as an extension of it, if only because I believe he will benefit from some R&R in response to whatever happened off-wiki today and in the meantime it will give @AlyInWikiWonderland something to consider Re:
| Biological target of amphetamine |
Secondary effector protein kinase |
Phosphorylated transporter |
Effect on transporter function | Effect on neurotransmission | Sources |
|---|---|---|---|---|---|
| Unidentified | CAMKIIα | DAT | Reverse transport of dopamine | Dopamine efflux into synaptic cleft | [52][53][54] |
| TAAR1 | ROCK† | DAT | Transporter internalization | Dopamine reuptake inhibition | [55][56][57] |
| TAAR1 | ROCK† | EAAT3 | Transporter internalization | Glutamate reuptake inhibition | [55][56][57] |
| TAAR1 | PKA | DAT | Transporter internalization | Dopamine reuptake inhibition | [58][59] |
| TAAR1 | PKC | DAT | Reverse transport of dopamine Transporter internalization |
Dopamine efflux into synaptic cleft Dopamine reuptake inhibition |
[53][58][59] |
| †Note: ROCK-mediated transporter internalization is transient due to the inactivation of RhoA (which activates ROCK) by PKA. | [60][56][57] | ||||
- Re:
TAAR1 knockout models
- The argument that TAAR1 KO models demonstrate TAAR1’s irrelevance ignores the fact that TAAR1 and D2 autoreceptors interact dynamically to regulate dopamine signalling. TAAR1-D2 heterodimerisation is eliminated in knockout models, and D2 receptor expression is markedly upregulated in the absence of TAAR1. These compensatory changes completely disrupt the normal dynamics of dopamine release and reuptake. As a result, TAAR1 KO experiments do not provide a controlled comparison of TAAR1 function. They do demonstrate how removing TAAR1 borks the balance of the release/reuptake system, though.
- With all that said, I can't think of anything else to add right now. I think I'm going to got take a nap and check back in on this either tomorrow or the day after. :P Professional Crastination (talk) 10:29, 14 December 2024 (UTC)
- agree with Seppi333(short but to the point)--Ozzie10aaaa (talk) 13:32, 14 December 2024 (UTC)
- Re:
- Thanks for the cordial and extensive reply User:Professional Crastination, I appreciate it. Your response helped clarify some important things for me about what you and User:Seppi333 are claiming. The main takeaway for me is that you two believe that amphetamine (and/or other MRAs) do not induce MAT monoamine efflux via TAAR1 alone but by multiple intracellular targets (e.g., TAAR1, unidentified target -> CAMKII, etc.). This is important since it would seem to explain, at least theoretically, (1) how amphetamine could continue to induce monoamine release (albeit seemingly less potently) without TAAR1 in vitro; (2) how amphetamine could still be active in TAAR1 KO mice in vivo (aside from additionally acting as a monoamine reuptake inhibitor); and (3) how other MRAs without hTAAR1 agonism could be active as MRAs in spite of lack of TAAR1 activation. This would seemingly obviate a few of my points. Would you and User:Seppi333 agree with that interpretation?
- I suppose then a critique I have is that this is not well-represented in the relevant content on Wikipedia in many places, like the dextroamphetamine, Adderall, lisdexamfetamine, and monoamine transporter pages (which make no mention of pathways other than TAAR1 such as CAMKII in their text, though CAMKII is mentioned in that transcluded figure). I feel like the relevant parts of these articles in general should start with something like "amphetamine appears to induce monoamine efflux via multiple known targets, including [...]". Right now, they start with TAAR1 agonism, and CAMKII is left almost as an afterthought. Relatedly, it's unclear to me why TAAR1 agonism should be highlighted as preferential, aside simply from its status of being of known identity. If many other MRAs are not hTAAR1 agonists yet are still very efficacious MRAs, if amphetamine is still such a robust releaser in TAAR1 knockout mice, and so on, then I feel like that all implies that the CAMKII pathway (and/or any other pathways) may be a lot more important and TAAR1 less so? Moreover, are there any other possible (known or unknown) pathways besides these two (for MAT monoamine efflux specifically)? As an example, I noticed that amphetamine and mephedrone have been implicated in mediating monoamine efflux through OCT3 (SLC22A3), and this seems to explain paradoxical synergy between MDPV and mephedrone.[32][61][62]
- Re:
TAAR1 is unequivocally a major intracellular target of amphetamine, [...]
. I understand that you and User:Seppi333 feel this way. And you might be correct. But this is an uncited assertion. What are the hard sources/evidence to show that this is true? I'm particularly preoccupied now with the micromolar EC50 values of amphetamine and methamphetamine at the hTAAR1, which are seemingly not compatible with TAAR1 agonism being a significant action of these agents at clinical doses in humans. Indeed, I've seen multiple papers imply that amphetamine and/or methamphetamine probably aren't significant TAAR1 agonists at therapeutic doses in humans but TAAR1 agonism might become significant in the context of methamphetamine addiction with extreme dose escalation and tolerance (resulting in far higher concentrations than usual that could potentially activate the TAAR1).[63][64] (It's notable that David K. Grandy is an author of these papers. He has also coauthored a relevant 2016 review with Miller.)[65] You can show that TAAR1 agonism produces monoamine release in vitro, but it's another thing to show that that's actually relevant in vivo.
- Re:
- Re: VMAT2, I mentioned above to User:Seppi333 that several notable MRAs are inactive at VMAT2 yet remain robust MRAs with effects similar to those of amphetamine and methamphetamine, for instance phenmetrazine. How do you explain this?
- Re: TAAR1 KO mice, yes, that does seem to make sense. And it makes more sense if amphetamine induces MAT monoamine release by multiple targets, not merely by TAAR1 agonism, because then it can still be active in KO mice. That said, an interesting study I came across has me questioning your explanation.[66] It found that TAAR1 KO amplified dopamine release and hyperlocomotion induced by MDMA (a TAAR1 agonist) relative to WT in vivo, as we see with (meth)amphetamine, whereas dopamine release induced by the closely related MRA para-chloroamphetamine (PCA) (not a TAAR1 agonist) was not different between TAAR1 KO and WT in vivo.[66] Moreover, addition of a TAAR1 agonist (o-PIT) to PCA blunted PCA-induced dopamine release both in vivo and in vitro in synaptosomes in WT mice, but not, of course, in TAAR1 KO mice, mirroring what was seen with MDMA on its own.[66] This study seems to suggest that TAAR1 agonism is not meaningfully involved in MRA induction of monoamine release in vivo and instead serves overall solely to inhibit it. Accordingly, the paper's title was "Genetic deletion of trace amine 1 receptors reveals their role in auto-inhibiting the actions of ecstasy (MDMA)". I also looked up cocaine in TAAR1 KO mice, and cocaine-induced locomotor activity (and presumably by extension dopamine elevation) was no different between TAAR1 KO mice and WT mice, similarly to the case of PCA.[67] Hence, it seems that it is specifically MRAs(/MRIs) acting as TAAR1 agonists that are affected by TAAR1 KO, not MRAs in general, and TAAR1 agonism by these agents is self-inhibiting.
- User:Seppi333, feel free to chime in on any of these as well. – AlyInWikiWonderland (talk, contribs)
- No worries. Glad to hear my reply was helpful. :)
- Re: "
"TAAR1 is unequivocally a major intracellular target of amphetamine, [...]". I understand that you and User:Seppi333 feel this way. And you may be correct. But this is an uncited assertion. What are the hard sources/evidence to show that this is true?
" - The citations are in the wikitable I posted. The data indicates that PKC is responsible for ~50% of DA efflux. The data also indicates that TAAR1-mediated PKA and PKC signaling cascades are involved in amphetamine-induced DA reuptake inhibition (i.e., transporter internilisation). With regard to DA efflux specifically, amphetamine induces a PKC signaling cascade via TAAR1 and another yet unidentified mechanism that then induces a CAMKII-alpha signalling cascade, with the former account for 50% of DA efflux. This citation attributes a specific percentage of dopamine efflux to a protein kinase. "
Consistent with this idea, PKCb knockout mice demonstrate reduced, though notably not completely eliminated, AMPH-evoked DA efflux (Chen et al., 2009). Similar results were recently observed by the Gnegy group, who found that perfusion of PKCb inhibitors into the nucleus accumbens of rats reduced AMPHevoked DA efflux by approximately 50% (Zestos et al., 2016).
"[54] - Moreover, this review indicates: "
The fact that TAAR1 is a direct, high affinity target for METH and AMPH whereas the DA D2R is not (Xie et al., 2007b) supports the idea that METH/AMPH interferes with TAAR1/DA D2R functional and/or physical interaction(s). ... The interpretation made of these data is that as a TAAR1 ligand/DAT substrate (i.e. METH/AMPH/DA) enters the cell via the DAT and accumulates, TAAR1 signaling progressively occurs. In turn, phosphorylation cascades are promoted ultimately modulating DAT kinetics.
"[59] - Re: "
I feel like the relevant parts of these articles in general should start with something like "amphetamine appears to induce monoamine efflux via multiple known targets, including [...]". Right now, they start with TAAR1 agonism, and CAMKII is left almost as an afterthought.
" - I'm not opposed to this and I think Seppi333 could be on board for this because they actually intended to make this change a few years ago. For context, at the end of 2019 Seppi had expressed desire to update amphetamine's pharmacology section to reflect the current (at the time) literature covering amphetamine's pharmacodynamics in DA neurons. The wikitable I linked above was Seppi's work and this table was to be added to supplement an updated graphic (i.e., the amphetamine pharmacodyanmics in dopamine neurons template). However, that hasn't come about yet and TMK that's because of two reasons. (1) I believe Seppi was waiting for the CAMKII-alpha cascade to be fully elucidated and (2) Seppi became seldom active on Wikipedia shortly after because I'm assuming he was motivated to prioritise his time toward the development of his new company. Furthermore, over the years no other editor - besides myself - has expressed an interest in majorly overhauling the amphetamine article in a manner that's consistent with its featured article status. I would certainly like to see an update to the pharmacology section with that table alongside the redrawn diagram template. Seppi previously drafted the following sentence as an appended note to the wikitable and I think something analogous to that would improve the article.
- "
Amphetamine interacts with its receptor protein target(s) (i.e., TAAR1 and a currently unidentified biomolecular target which initiates its CAMKIIα cascade), which triggers the activation of protein kinases. The activated kinases then phosphorylate their respective transporter(s), which in turn causes a conformational change in transporter protein, thereby altering its function and affecting dopaminergic/glutamatergic neurotransmission at dopaminergic synapses.
" - I'm happy to work on updating/redrawing the SVG of the amphetamine pharmacodynamics template sometime over the next week/the holiday season. This would likely be based on the figure in this paper[55]; i.e., the RhoA signalling cascade would be drawn from TAAR1 and the CAMKII-alpha signalling cascade will likely involve appending an "Unidentified intracellular pathway" figure before drawing the pathway to DAT to illustrate that it confers DA efflux. I'll also have add glutamatergic pharmacodynamics of amphetamine in DA neurons (i.e., EAAT2 internalisation and VGLUT2 in the axon terminal). Professional Crastination (talk) 12:40, 16 December 2024 (UTC)
- User:Seppi333, feel free to chime in on any of these as well. – AlyInWikiWonderland (talk, contribs)
I appreciate you reposting that table Professional Crastination; I actually forgot about that.
Anyway, I'll address a few points: I really don't know or care about most structural analogs of amphetamine. Structure activity relationships only go so far, and drugs like cathinones have virtually nothing in common with amphetamine in a pharmacodynamic sense despite having amphetamine in its structural backbone. Even just N-methylating amphetamine changes some of its downstream targets from TAAR1 and the VMAT2 binding site; tacking more crap onto that backbone like a methylenedioxy group would only introduce further changes. But, monoamine-releasing agents are simply a drug class that shares a common mode of action, not a common chemical structure or a common mechanism of action that mediates said mode. That's why I don't care to comment on that point. I simply know close to nothing about most MRAs, which is a very large drug class.
Pharmacodynamics of amphetamine in a dopamine neuron
|
As for amphetamine and TAAR1, yes the relationship there is paradoxical. But the same is true for amphetamine and VMAT2. Amphetamine binds at the tetrabenazine binding site on the latter protein. What does tetrabenazine do, though? Well, it effectively sequesters most vesicular dopamine within the cytosol of a neuron, where it just gets broken down because it's not being pumped out through a transporter or dumped into the synapse within a vesicle. As for selective TAAR1 full agonists? Well sure, they induce reverse transport and reuptake inhibition at transporter proteins, but unless there's a ton of dopamine within the neuronal cytosol, that mechanism of action is not going to induce any notable monoamine release; they're not like amphetamine at all. Amphetamine's activity at TAAR1 and VMAT2 individually is actually strongly inhibitory in dopamine neurons, which is exemplified by drugs that selectively interact with those proteins; but, the combination of those two mechanisms strongly promotes monoamine release. There is very likely another intracellular target of amphetamine that mediates reverse transport at DAT, but it's not required for it to act as an MRA. Seppi333 (Insert 2¢) 19:20, 14 December 2024 (UTC)
- I would argue that you should care about other MRAs though. Because they're closely structurally related to amphetamine, surely have substantial overlap with the mechanisms of amphetamine, and can provide indirect insights into amphetamine's pharmacology. Personally I think the lack of hTAAR1 agonism with many of them should be telling in terms of weighing the likely relative significance of TAAR1 agonism versus other mechanisms to monoamine release induced by amphetamine. Does that not make you think for a moment too? Relatedly, you could also argue something similar about the importance of VMAT2 in monoamine release with amphetamine and other MRAs (see what I wrote about VMAT2 above).
- On this topic of other MRAs, I'd like to also note that this TAAR1 agonism theory of MRA monoamine release has been applied to other MRAs on Wikipedia, for instance at monoamine releasing agent, TAAR1, MDMA, phentermine, and propylhexedrine among others. I don't know if that was always you or others. And it might of course prove to be valid in some cases. But obviously applying TAAR1 agonism as the mechanism of monoamine release to MRAs in general needs to be considered with significant nuance. I do not think it's likely to apply to MDMA for instance and that content should be corrected.
- I should note that I'm not mystified by the fact that selective TAAR1 agonists don't have amphetamine-like effects. The need for concomitant MAT uptake (and, per you, VMAT2 activity) aspect of things has made sense to me there. While amphetamine (and other sufficiently lipophilic TAAR1 agonists) can passively diffuse into cells, active transport by MATs appears to dramatically increase its passage.[48] This, in turn, will result in a very different pattern or distribution of TAAR1 signaling in the CNS, and by extension the potential for very different effects. At least on a theoretical level and assuming the TAAR1 MRA theory is true. It's more all of the other points I mentioned that have given me pause.
- Besides the other things I mentioned above, I'm also still quite concerned about the fact that the amphetamine TAAR1 MRA theory appears to be very obscure and not well-established or widely accepted. Looking to get some more insight, I emailed Dr. David Sulzer at Columbia University today. He is the originator of the "weak base theory", is one of the world's leading experts on amphetamine pharmacology (or perhaps the leading expert, per Hamilton Morris),[74] and is the lead author of a major 2005 review on mechanisms of amphetamine-induced monoamine release.[75] He had never heard of TAAR1 mediating amphetamine-induced monoamine release before. I showed him the Miller and Xie studies and asked him what he thought about them and the theory. He said they were interesting. But he looked up TAAR1 KO studies by his own accord and discounted the theory. He said that you should read more of the well-accepted literature on this topic and provided two of his reviews, one of which was the 2005 review (which he said was mostly accurate but outdated due to lacking Paul Phillip's more recent findings).[75][76] Along similar lines, a very relevant 2024 review, "Post-Translational Mechanisms in Psychostimulant-Induced Neurotransmitter Efflux", barely mentions the TAAR1.[77] Same again for a 2020 review by Maarten Reith (another well-known expert on MRAs) and colleagues, "Molecular Mechanisms of Amphetamines"—it implicated DAT, VMAT2, and OCT3, as well as PKC, CaMKII, and ERK, but no mention of TAAR1 at all.[48] These are major recent literature reviews on amphetamine mechanisms and yet they barely mention TAAR1, which you assert is the key mediator of amphetamine actions.
- I've only implied this before, but Wikipedia policy dictates that content should, of course, reflect mainstream scientific views and consensus:
- "In Wikipedia parlance, the term fringe theory is used in a broad sense to describe an idea that departs significantly from the prevailing views or mainstream views in its particular field. Because Wikipedia aims to summarize significant opinions with representation in proportion to their prominence, a Wikipedia article should not make a fringe theory appear more notable or more widely accepted than it is. Statements about the truth of a theory must be based upon independent reliable sources. If discussed in an article about a mainstream idea, a theory that is not broadly supported by scholarship in its field must not be given undue weight,[1] and reliable sources must be cited that affirm the relationship of the marginal idea to the mainstream idea in a serious and substantial manner." (WP:FRINGE)
- It does not currently appear to be scientific consensus, let alone even well-known, that TAAR1 agonism mediates MRA actions of amphetamine and that this is relevant in humans. It's an obscure and limitedly supported theory. And a theoretical possibility that indeed might have merit, sure. But clearly more research seems necessary to demonstrate that it has basis. Miller himself, the originator of the idea, has shown due restraint in this regard in his publications, as would be expected of any rigorous scientist; from a 2016 review he coauthored: "That TAAR1 signaling is coupled to the inhibition of VTA DA neuron firing was a surprising finding. [...] Nonetheless, this mismatch in expectations immediately attracted the attention of those trying to determine whether TAAR1 is a METH/AMPH and DA receptor in vivo as it is in vitro (Bunzow et al., 2001; Wainscott et al., 2007; Xie and Miller, 2009; Panas et al., 2012)."[65] I'm currently conversing with Miller by email and getting his take on things as well. He has expressed that these in-vitro findings are highly methodology-dependent and you can potentially obtain even opposite results with different in-vitro systems and techniques (due, e.g. and among other factors, to TAAR1-mediated DAT internalization being inhibitory not only of reuptake but also of efflux). In turn, he has placed a great deal of value on in-vivo research, for instance with KO mice as well as canines (which notably lack a functional TAAR1[78]).
- Based on all of this, I think that the current content on Wikipedia re: TAAR1 agonism being the mediator of the monoamine release of amphetamine and other MRAs needs to be presented much more conservatively. Because right now people reading it will just assume that it's definitively how amphetamine and other MRAs work, and that is not currently what the literature reflects. I think the content should say something like "The mechanisms of amphetamine-/MRA-induced monoamine release are unknown. [...] TAAR1 agonism (also CAMKII) is one possible contributing factor based on in-vitro studies. In any case, more research is needed." (Not verbatim. Just a very rough idea or start.) That kind of approach would be much more true to the current scientific literature. – AlyInWikiWonderland (talk, contribs)
- TAAR1 agonism is a mechanism of action for any MRA even for selective full agonists; it's just not that notable as I said before. It is well established in every review and primary source that's been cited. Is it the primary mechanism of action? Perhaps not for some drugs like phentermine, which isn't really a releasing agent at all. But, until you can substantiate your theory that TAAR1-mediated PKCβ-induced DAT reverse transport insignificantly affects DA efflux relative to CAMKIIα, this is a moot point to argue given that there is no evidence to support that assertion. Seppi333 (Insert 2¢) 10:35, 16 December 2024 (UTC)
- But hey, if you really want to test it in vivo, buy a selective full hTAAR1 agonist and tetrabenazine from sigma aldrich and take them both, then you'll know whether you're right. Seppi333 (Insert 2¢) 11:01, 16 December 2024 (UTC)
- I have to go for now, but I wanted to leave something here before I do. Another study recently attempted to replicate Xie & Miller's findings on methamphetamine in vitro and failed to do so:[79]
- "Previous research on TAAR1 modulation of DAT function has produced equivocal findings. In vitro, MA inhibits [3H]DA uptake, and [3H]DA release is increased in striatal tissue from Taar1 WT compared with KO mice (Xie and Miller, 2009). Similar findings were described in cells cotransfected with TAAR1 and DAT, compared with cells transfected only with DAT, in which MA-induced [3H]DA uptake inhibition and release were increased (Xie and Miller, 2007, 2009). However, these findings indicate MA-induced impairment of DAT function is increased when TAAR1 is activated, as opposed to in vivo treatment with AMPH or MDMA, by which striatal extracellular DA levels are increased when TAAR1 is not activated (Wolinsky et al., 2007; Lindemann et al., 2008; Di Cara et al., 2011). We were unable to replicate the results of Xie and Miller (2009) under similar in vitro conditions (Fig. 3). There was no difference in IC50 values for [3H]DA uptake inhibition by MA between synaptosomes from Taar1 WT and KO mice. [...]
- [...] our results do not support an earlier hypothesis that TAAR1 modulates DAT (Xie and Miller, 2007, 2009; Xie et al., 2008b), as there was no evidence of an interaction under conditions described above. Recent reports support our findings that the DAT is unaffected by TAAR1. Coadministration of MA and the TAAR1 partial agonist RO523648 did not alter [3H]DA uptake and release in striatal synaptosomes in rats (Cotter et al., 2015). Fast-scan cyclic voltammetry showed no difference in DA clearance, as mediated by DAT, in striatal tissue from Taar1 WT compared with KO mice (Leo et al., 2014). Finally, selective TAAR1 agonists diminished hyperlocomotion in DAT KO mice and DAT KO rats, providing behavioral evidence that TAAR1 signals independently of DAT (Revel et al., 2011; Leo et al., 2018). Given the lack of interaction, DAT is an improbable mediator of TAAR1 regulation of MA-induced neurotoxicity.
- [...] activation of TAAR1 did not modulate in vitro MA-impairment of DAT function or DAT expression. As TAAR1 activation did not alter the function or expression of DAT in whole synaptosomes or VMAT2 located on membrane-associated vesicles, these results indicate TAAR1 does not interact with these transporters on the plasma membrane but does affect intracellular VMAT2 function."
- I really don't know how you could continue to assert this theory with so much counterevidence. I have also reached out to Dr. Maarten Reith and asked him his opinions about the TAAR1 agonism theory. We'll see what he says as well. I suspect he did not include the TAAR1 agonism theory in his 2020 review because there are so many findings that overtly contradict it (particularly the TAAR1 KO studies). At this point, I really think you need to concede that your theory is highly uncertain, that it is not scientific consensus or widely accepted, and that the current content on Wikipedia needs to be refactored.
- I'll respond to the rest of the comments here later. – AlyInWikiWonderland (talk, contribs)
- I've been going through the literature and have found further findings contradicting the results of Miller & Xie.
- Leo, Mus, & Espinoza (2014):[80]
- "Importantly, we have documented that neither Tau nor the half-life of released DA are changed in slices from TAAR1-KO animals, indicating that TAAR1-KO mice exhibit unaltered DA uptake ability and thereby normal dopamine transporter (DAT) functionality. It is believed that Tau and the half-life of released DA are reliable measures for detecting changes in DA uptake because they are strongly correlated with changes in the Km of DAT mediated DA uptake (Yorgason et al., 2011). Thus, these neurochemical in vivo studies, as well as previous demonstrations of the functional activity of TAAR1 ligands in mice lacking the DAT (Sotnikova et al., 2004; Revel et al., 2012a), provide little support for the postulated role of TAAR1 in modulating DAT activity that is based mostly on in vitro cell culture experiments (Miller et al., 2005; Xie et al., 2008; Miller, 2011). [...] Notably, neither [the TAAR1 agonist (RO5166017) nor the TAAR1 antagonist (EPPTB)] changed the kinetics of DA uptake as evidenced by the Tau and DA half-life estimations, indicating that DAT-mediated function is not altered by the action of the drugs on TAAR1."
- Rutigliano, Accorroni, & Zucchi (2018):[81]
- "Evidence of a reciprocal regulation of monoamine transporters by TAAR1 came from in vitro experiments, where it was found that pretreatment with dopamine, serotonin, NE, and methamphetamine significantly inhibited monoamine uptake in HEK293 cells co-expressing TAAR1 and DAT/SERT/NET (Xie and Miller, 2007, 2009), a finding that was later confirmed in synaptosomes (Xie et al., 2008b; Xie and Miller, 2009). [...] The observed regulatory actions of TAAR1 on transporters are supposedly dependent on cAMP accumulation and PKC-phosphorylation, as they were prevented by the PKC inhibitor Ro32-0432 (Xie and Miller, 2007, 2009; Xie et al., 2008b). [...] However, TAAR1-KO and wild-type mice showed overlapping dopamine uptake and half-life, indicating normal DAT activity (Leo et al., 2014), consistent with unaltered in vivo functional activity of TAAR1 agonists over the behavioral abnormalities of DAT-KO mice (Giros et al., 1996; Sotnikova et al., 2004; Revel et al., 2012). On the whole, the relevance of TAAR1 interaction with brain monoamine transporters still awaits clarification (Figure 5)."
- Miner (2019):[82]
- A significant body of in vitro research has investigated TAAR1 modulation of DAT, primarily by the Miller laboratory. [...] Functionality of DAT is also modulated by TAAR1 as application of DA inhibited [3H]DA uptake and induced [3H]DA release in TAAR1/DAT cells compared to cells only expressing DAT (Xie and Miller, 2007; Xie et al., 2008b). [...] However, it has been argued the conduction of this research in vitro diminishes its validity. Administration of β-PEA or the TAAR1 agonist RO5166017 diminishes hyperlocomotion in DAT-KO mice, indicating activation of TAAR1 functions independently of DAT (Sotnikova et al., 2004; Revel et al., 2011). This theory is bolstered by FSCV experiments. Evoked DA release and uptake, measured by Tau and half-life, are the same between genotypes. DA overflow is greater in the NAc of Taar1-KO than -WT mice, attributed to increased basal DA levels, but DA uptake is still the same between genotypes (Leo et al., 2014). Similarly, the partial TAAR1 agonist RO5203648 diminishes cocaine-induced DA overflow in the NAc without altering DA uptake, also indicating a DAT-independent mechanism (Pei et al., 2014). Further research is needed to better elucidate the interaction between TAAR1 and DAT.
- Jing & Li (2015):[24]
- "There [is] evidence that TAAR 1 can modulate DAT function in in vitro cell culture experiments. Xie et al reported that β-phenethylamine (β-PEA) inhibited uptake and induced efflux of monoamines in thalamic synaptosomes of rhesus monkeys and wild-type mice, but not in synaptosomes of Taar 1−/− mice. Furthermore, the effect of β-PEA on efflux was blocked by transporter inhibitors in either the transfected cells or wild-type mouse synaptosomes (Xie and Miller, 2008). They also found that methamphetamine inhibited DA uptake, enhanced dopamine efflux, and induced DAT internalization by acting as a TAAR 1 agonist (Xie and Miller, 2009). However, more recent studies show inconsistent results. Leo et al. found that the DA clearance was not changed in Taar 1−/− mice as compared to their wild type counterparts (Leo et al., 2014), suggesting that the DAT function remained intact. In addition, no significant changes of dopamine uptake were observed in slices from Taar 1−/− mice, suggesting that the effect of TAAR 1 activation on DA-related function is independent of DAT (Leo et al., 2014). These apparent discrepancies may be attributable to the assays and tissues used in the studies. Xie et al. used mouse and monkey cellular synaptosome preparations with tissues from putamen and thalamus (Xie and Miller, 2008) while Leo et al. used fast scan cyclic voltammetry to measure DA uptake in mouse striatal slices (Leo et al., 2014)."
- Wu & Li (2021):[25]
- "The role of TAAR1 in the dopaminergic system has been further characterized by studies that examines its interaction with dopamine transporter (DAT) and dopamine receptors. DAT is important for dopamine transmission as it mediates the reuptake of released dopamine back to the presynaptic terminals and thus is closely associated with the psychostimulant effects of METH [45–48]. TAAR1 was found to be co-expressed with DAT in dopamine neurons in both the primates and the mice [49] and in vitro co-expression of TAAR1 with DAT significantly enhanced TAAR1 signaling in a DAT-dependent manner [49, 50]. Furthermore, TAAR1 modulation of dopamine reuptake and efflux may be dependent on the activities of protein kinase C (PKC) and protein kinase A (PKA) [51]. However, in other studies, no changes were observed with respect to dopamine reuptake in TAAR1-KO mice nor after TAAR1 alterations in WT mice [52]. TAAR1 agonists are also able to inhibit dopamine-related hyperlocomotion in DAT-KO mice [38, 40, 53]. Therefore, it appears that the effect of TAAR1 on dopamine transmission may occur in a DAT-independent manner."
- Li (2017):[83]
- "Increasing evidence suggests that TAAR 1 has a close interaction with dopamine transporters (DAT) and dopamine D2 receptors. TAAR 1 is coexpressed with DAT in a subset of dopamine neurons in both rhesus monkey and mouse substantia nigra (Xie et al., 2007) and accumulating evidence suggests a dynamic interaction between TAAR 1 and DAT. The trace amine β-phenethylamine inhibits uptake and induces efflux of monoamines in thalamic synaptosomes of rhesus monkeys and wild-type mice, which is blocked by monoamine transporter inhibitors in either the transfected cells or wild-type mouse synaptosomes (Xie & Miller, 2008). Importantly, methamphetamine can inhibit dopamine uptake, enhance dopamine efflux, and induce DAT internalization by acting as a TAAR 1 agonist (Xie & Miller, 2009), suggesting the direct involvement of TAAR 1 in methamphetamine pharmacology. In TAAR 1 knockout mice, the dopamine clearance and reuptake remains relatively normal, which is inconsistent with the above results (Leo et al., 2014), and the causes of such discrepancies are uncertain with the different tissues and bioassays used being potential culprits."
- Liu et al. (2022):[84]
- "Previous in vitro studies showed that TAAR1 activation stimulated several signaling cascades, including PKA, PKC, ERK1/2, and CREB [13, 38]. For example, a recent study showed that intracellular TAAR1 mediated the effects of amphetamine, a TAAR1 agonist, on RhoA and PKA signaling through G13 and to GS α-subunits on the midbrain slice of mice [39]. However, our present [in-vivo] study showed that the TAAR1 agonist RO5166017 did not affect the activities of PKA, PKC, ERK1/2, CREB, or GSK3β, but selectively inhibited CaMKIIα in the NAc of rats. The discrepancies could be due to differences between in vitro and in vivo microenvironments."
- "Here, we tested in rats the ability of RO5203648, a selective TAAR1 partial agonist, to modulate the physiological and behavioral effects of methamphetamine (METH). [...] Neurochemical data showed that RO5203648 did not affect METH-mediated DA efflux and uptake inhibition in striatal synaptosomes. [...] In the synaptosomal preparation RO5203648 did not affect METH-induced striatal DA release and DA uptake inhibition, suggesting that RO5203648 regulation of METH’s behavioral effects is unlikely to depend on direct, local actions at the DAT.
- And finally, Di Cara, Maggio, & Aloisi (2015) (that TAAR1 MDMA and PCA study)[66] directly contradicts Miller & Xie's results as well. They found that the TAAR1 agonist o-PIT by itself had no effect on monoamine release in synaptosomes and that it suppressed monoamine release induced by PCA in synaptosomes, an effect that was absent in synaptosomes from TAAR1 KO mice.[66] (Note that Miller & Xie's findings on TAAR1 mediation of amphetamine MAT efflux and reuptake inhibition were likewise primarily done with synaptosomes.)
- So yeah, not only did Miner, Phillips, & Janowsky (2019)[79] fail to replicate Xie & Miller's findings, but multiple other groups of researchers have contradicted and expressed doubt about their findings as well. You can add this all to the pile of TAAR1 mediation of amphetamine MRA actions not being scientific consensus nor widely accepted. – AlyInWikiWonderland (talk, contribs)
- User:Seppi333: I'm only going to respond to this part of your comments:
It is well established in every review and primary source that's been cited.
That isn't the same thing as following scientific consensus or appropriately representing mainstream scientific views. Which, again, Wikipedia policies require. TAAR1 agonism mediation of amphetamine actions is your personal preferred theory of how amphetamine works. A rather obscure theory that is based on the in-vitro findings of a single lab, which other researchers haven't been able to replicate and which have been contradicted by many other studies and findings. This theory should not be presented as fact all over Wikipedia in the way that it currently is. – AlyInWikiWonderland (talk, contribs)
- User:Seppi333: I'm only going to respond to this part of your comments:
User:Professional Crastination: Responding to your comment down here. I appreciate your response and explanations.
Respectfully, I don't feel that the provided sources show that TAAR1 is unequivocally a major intracellular target of amphetamine.
The Bermingham & Blakely (2016) review you cited indeed implicates PKC activation as mediating a substantial portion of amphetamine-evoked dopamine efflux.[54] However, Bermingham & Blakely (2016) make no mention of TAAR1 in their review.[54] It's the same with the Wang et al. (2016) study from the wikitable, which implicates PKC activation amphetamine-induced monoamine efflux but makes no mention of TAAR1.[53]
The Reith & Gnegy (2020) review I've cited elsewhere on this talk page implicates PKC activation in amphetamine-induced monoamine release similarly to your sources.[48] However, again, there is no mention of TAAR1.[48] Same with the Vaughan et al. (2024) review I've cited as well.[77] It appears that PKC activation as a mediator of amphetamine's MRA actions is well-established and accepted, going back to 1992 and having been substantiated by many independent studies.[48] But, as far as I'm aware, it's only the Miller group, based on their in-vitro synaptosome (and transfected cell-line) studies, that is claiming that TAAR1 is responsible for amphetamine-induced PKC activation and consequent monoamine efflux.
In contrast to these claims, Reith & Gnegy (2020) state the following rather than implicate TAAR1: "The most parsimonious explanation for the activation of PKC in response to amphetamine is the amphetamine-stimulated elevation of cytosolic Ca2+ in the nerve terminal.
"[48] Moreover, Sulzer (2016) states the following: "2.2.1. DAT regulation by psychostimulants [...] While several kinases are involved in the regulation of DAT, PKC is by far the most thoroughly investigated [388,403]. PKC activation induces DAT internalization [393,404–406] although the mechanism of PKC activation by DAT substrates remains largely unknown [388,389,403,407,408].
"[85] (Recall that Sulzer has been referred to as perhaps the world's leading expert on amphetamine pharmacology.[74])
The second review you cited is by Miller and just reviews their in-vitro synaptosome/cell-line findings. These findings are obscure and other researchers have been unable to replicate their results (see my last comments to User:Seppi333). Moreover, there is no evidence for amphetamine-induced monoamine efflux being mediated by TAAR1 in vivo (even in animals) that I'm aware of. It isn't widely accepted that TAAR1 mediates amphetamine-induced PKC activation and monoamine efflux and instead the mechanisms are unknown. I feel that the article needs to reflect this.
That's interesting that you and User:Seppi333 have had plans to majorly overhaul the amphetamine article (or its pharmacology section at least). I agree with that, but obviously I disagree on the specifics. In any case, I'd potentially be willing to help with some of the revisions. I'm not convinced that consensus couldn't be reached. – AlyInWikiWonderland (talk, contribs)
User:Seppi333: One last thing to note. I went through all of the Xie and Miller studies finding TAAR1-mediated induction of monoamine efflux. None of them actually employed amphetamine or d-amphetamine. They all used (d-)methamphetamine or phenethylamine (as well as dopamine, norepinephrine, and serotonin). You say that you only know how amphetamine works. And you say that you don't know how any other MRAs work, even MRAs with only one- or two-substituent differences from amphetamine (e.g., cathinones, MDMA, etc.). But your theory about amphetamine is actually a generalization from findings with other MRAs (i.e., methamphetamine, phenethylamine, etc.). Granted, amphetamine is a TAAR1 agonist with similar potency as methamphetamine, and the generalization certainly isn't unreasonable. But I wanted to make note of this nonetheless, since (1) the amphetamine and related articles like dextroamphetamine make a claim that has never actually been scientifically demonstrated for amphetamine itself; and (2) because you've emphasized so much about not extrapolating from other MRAs. – AlyInWikiWonderland (talk, contribs) 13:31, 19 December 2024 (UTC)
- Lol. I just spent like three hours writing a reply, then my computer blue screens and I lose everything.
- AlyInWikiWonderland,
You say that you only know how amphetamine works.
DON'T PUT FUCKING WORDS IN MY MOUTH. I want you to link a diff right now. - It's pretty clear you don't understand how Wikipedia works. This is a massive thread I no longer wish to read because this is all you and your opinion as a fake scientist. You have some idea in your mind as to how all this shit works from reading a bunch of papers. Great. It's fine if the authors we cite generate a pharmacodynamic model. Doing it as an editor is blatant WP:SYNTH.
- I'm sick and busy as fuck this week. Considering that and the fact that I just wasted 3 hours of my time to respond to some complete random I met on the internet who just implied that I believe I have some unique, specialized understanding of a drug which no one else has, well, that pisses me off.
- FWIW, "
So yeah, not only did Miner, Phillips, & Janowsky (2019) fail to replicate Xie & Miller's findings, but multiple other groups of researchers have contradicted and expressed doubt about their findings as well. You can add this all to the pile of TAAR1 mediation of amphetamine MRA actions not being scientific consensus nor widely accepted. – AlyInWikiWonderland (talk, contribs)
User:Seppi333: I'm only going to respond to this part of your comments: It is well established in every review and primary source that's been cited. That isn't the same thing as following scientific consensus or appropriately representing mainstream scientific views. Which, again, Wikipedia policies require. TAAR1 agonism mediation of amphetamine actions is your personal preferred theory of how amphetamine works. A rather obscure theory that is based on the in-vitro findings of a single lab, which other researchers haven't been able to replicate and which have been contradicted by many other studies and findings. This theory should not be presented as fact all over Wikipedia in the way that it currently is. – AlyInWikiWonderland (talk, contribs)".}} That's all just noise coming from someone on a crusade. I don't know how you acquired these fucking weird views of how I think about amphetamine's pharmacodynamics, but I don't care.[Edit: redacting my reply due to the misunderstanding stated below. Seppi333 (Insert 2¢) 21:53, 19 December 2024 (UTC)]- I'm out until Sunday at the earliest. Amphetamine isn't going to change unless you start linking a pharmacodynamic model you didn't invent yourself. You are not a reliable source for Wikipedia and you never will be. Seppi333 (Insert 2¢) 14:05, 19 December 2024 (UTC)
DON'T PUT FUCKING WORDS IN MY MOUTH. I want you to link a diff right now.
You said this earlier in the discussion:Again, the only thing I really know is how AMPHETAMINE works, not MRAs in general
([1]). I interpreted what you said as conceding on all MRAs besides amphetamine (and the few others that Miller et al. studied).
- To be clear, you don't know anything about me. In any case, it's true that I'm not an expert nor academic in this area. That's why I contacted actual scientists and experts on amphetamines and MRAs, like Sulzer, and asked them about this theory. And they told me that they'd never even heard of it and that it was not well-accepted. Moreover, recall that it was Baggott's criticisms of the theory and the content on Wikipedia that motivated me to act in the first place. You are not above these academics. And you aren't above me either, for that matter.
It's fine if the authors we cite generate a pharmacodynamic model. Doing it as an editor is blatant WP:SYNTH.
This is a talk page. I've been trying to look at things through the lens of your model, which is not widely accepted, and see both how it could work and how it couldn't work given various things we know. Entertaining the theory like that was frankly being considerate on my part. If I were writing actual Wikipedia content, I'd just cite high-quality (and well-accepted) sources and re-state exactly what they say. For instance those Sulzer,[75][76][85] Reith,[48] and Vaughan[77] reviews. These are broad and independent reviews on the relevant subject matter. The Miller reviews are not.
- I am dedicated to this matter because I really dislike misinformation. And because this content has been up on Wikipedia for many years and it isn't going to stop bothering me until it's corrected. Note in any case that I am not the first to disagree with you about this theory (see Baggott above, also [2], [3], [4], etc.). It looks like at one point you were even pursuing having the monoamine releasing agent page/category in some capacity replaced with a TAAR1 agonist page/category ([5]). In spite of the fact that TAAR1 agonism as the mechanism of action of MRAs is not scientific consensus and dozens of known MRAs have no TAAR1 agonism. This seems like clear WP:ADVOCACY to me.
Amphetamine isn't going to change unless you start linking a pharmacodynamic model you didn't invent yourself.
I have no theoretical model of my own. This claim is a strawman argument. All I know is that there are numerous problems with the TAAR1 agonism theory that's being presented on Wikipedia. It isn't widely accepted or scientific consensus, it's based on the results of a few in-vitro studies by one lab that are largely or completely unreplicated, it's contradicted by many other findings, and it doesn't work for many MRAs closely related to amphetamine. I know that you know that these things are true. I wish that you would just admit it and we could move on and fix the content. I'm intent on having the relevant Wikipedia content corrected. I would defer to high-quality reviews on amphetamine mechanisms in terms of exactly what those corrections should look like. For example, I would change the amphetamine article to say that the mechanism by which amphetamine mediates PKC activation and consequent monoamine efflux is unknown (citing e.g. the Sulzer (2016) review[85]). And I would include that TAAR1 agonism is one possible mechanism per some studies but more research is needed. I'm fine with still mentioning the TAAR1 agonism theory in articles. I just want the content to be balanced and to reflect what the mainstream scientific view actually is. This isn't a huge ask.
- Take as much time as you need on responses. It's the holidays and it's not my intention for you to feel like there's pressure on you. I'm not going to touch the amphetamine article unless and until there's consensus. Sorry also if I'm a bit thorough and verbose. It's just how I am and can't really be helped. – AlyInWikiWonderland (talk, contribs) 16:32, 19 December 2024 (UTC)
- AlyInWikiWonderland: I wholeheartedly apologize for saying, "DON'T PUT FUCKING WORDS IN MY MOUTH. I want you to link a diff right now." I was half-asleep and already irritated from the pointless loss of 3 hours of time/effort I spent writing my original response. What I thought you wrote this morning when I misread the statement was "
You say that [only you] know how amphetamine works
", which is something that only an imperious piece of shit would say. What you actually wrote is indeed exactly what I originally said. "You say that you only know how amphetamine works
." My bad for getting so triggered, but that's what I thought you meant when I stated, "who just implied that I believe I have some unique, specialized understanding of a drug which no one else has, well, that pisses me off." - If you want to give me a preferably–not–massive reading list of reviews that you think make a good argument that the pharmacodynamic model in the amphetamine article is wrong, I'll read them with intellectual honesty when I have time to spare this weekend. Once I'm caught up, that would be the best time to continue this discussion because we'll finally be on the same page.
- That said, the pharmacodynamic model is not technically mine; it's literally just Miller's model with VMAT2 included in the diagram. Seppi333 (Insert 2¢) 21:47, 19 December 2024 (UTC)
- AlyInWikiWonderland: I wholeheartedly apologize for saying, "DON'T PUT FUCKING WORDS IN MY MOUTH. I want you to link a diff right now." I was half-asleep and already irritated from the pointless loss of 3 hours of time/effort I spent writing my original response. What I thought you wrote this morning when I misread the statement was "
- Hi AlyInWikiWonderland
- I appreciate the time and effort you've dedicated to dissecting the literature on this topic. It’s clear to me that you’re genuinely committed to reaching a consensus that improves the article, and your thoroughness is something I really appreciate on Wikipedia (even if it comes at the cost of being in the running for the longest written WP:Pharmacology talk thread because Seppi333and I also have a tendency to produce essays on talk pages, but I don't think this thread be on the podium for longest talk page thread in general; I suspect that title belongs to a thread somewhere deep in the Talk:Circumcision archives ¯\_(ツ)_/¯). I’d be more than happy to collaborate with you not only on this article but on other topics down the line, even if they’re not necessarily amphetamine-related.
- Before I continue, I will be frank in saying that this reply might not contribute as much as I’d like. That's largely because I've had to pick up some extra, longer shifts at the hospital over this week. I also happen to take IR prescription amphetamine - which is ironic because it also happens to be the main topic of discussion - and as I'm sure you know from reading the article, the effects of that particular formulation are relatively transient; by the time I get home from work and attend to all my menial human maintenance tasks (e.g., cooking dinner, meal preparing for tomorrow, etc.), my third dose for the day has likely worn off and has rendered me to a state of being half-baked. So, to be transparent I haven't actually read any of the papers you've introduced in your recent reply. In any event, the reason I opened this reply with a compliment is because I am impressed and wish to express that I am open to taking you at face value, at least until my next day off where I can sit down and inspect everything closely and/or Seppi replies with something that validates TAAR1's involvement in amphetamine's monoamine efflux action in light of what you've presented. FWIW, I'm more reciprocal now since you've shared that the
TAAR1 --> cAMP --> PKC
signalling cascade that was believed to precede phosphorylation of DAT/SERT to confer monoamine efflux hasn't been replicated by other labs, especially if they're using analysis methods that are comparable to Miller. After all, as humbling as it is it's true that no one is completely infallible - Also, as an aside, is there any chance you'll forward me the emails you've received from Miller and Selzer (Miller is especially of interest)? I do trust that you've emailed them and have received the responses you've described, so I want you to know that I'm not asking because I have an issue with verifiability (after all, I'm assumming that you're aware that emails wouldn't meet WP:RS and you've emailed them simply because they're individuals with more experience in the field who may be able to help guide you to use your time productively when conducting you lit search on PubMed et. al for this thread; one example is when I emailed Eric Nestler to ask about a change to a Meth direct toxicity statement across revisions of his textbook). My email is
102559588@student.swin.edu.au
. If you don't wish to forward the emails to me because of privacy concerns (e.g., you wish to avoid sharing your name in the "from:" row), then I'm fine to leave the emails be; I only wish to read them out of curiosity. - With all that said, at this point I'm pretty optimistic that we'll be able to reach a resolution for the amphetamine article leading into 2025. =D Professional Crastination (talk) 08:55, 21 December 2024 (UTC)
That makes sense. No worries, mistakes happen. Thank you for the apology. Sorry for getting a little heated myself.
For sure. That sounds great! That's actually been a task I've been wanting to do, identifying the major reviews in this area.
I ended up doing the following PubMed query: (amphetamine* OR methamphetamine* OR dextroamphetamine*) (pharmaco* OR mechanis*) (transporter* OR "DAT")
, with reviews filter on and with date range from 2010 to present ([6]). The (transporter* OR "DAT")
part was to help reduce the number of results, which otherwise would've been overwhelming (around 20 times as many). I looked through the results and selected the ones that seemed highly relevant. Then I further filtered them by checking whether they substantively discussed PKC and hence are really about the mechanisms underlying amphetamine-induced DAT efflux that we're interested in. These are the resulting reviews (sorted by recency):
- Vaughan, R. A., Henry, L. K., Foster, J. D., & Brown, C. R. (2024). Post-Translational Mechanisms in Psychostimulant-Induced Neurotransmitter Efflux. In Gnegy, M. E. (Ed.). Pharmacological Advances in Central Nervous Stimulants (Advances in Pharmacology, Volume 99) (pp. 1–33). San Diego: Academic Press. [PubMed] [DOI:10.1016/bs.apha.2023.10.003] [Google Books]
- Reith, M. E. A., & Gnegy, M. E. (2020). Molecular Mechanisms of Amphetamines. In Nader, M. A., & Hurd, Y. L. (Eds.). Substance Use Disorders: From Etiology to Treatment (Handbook of Experimental Pharmacology, Volume 258) (pp. 265–297). Cham: Springer. [PubMed] [DOI:10.1007/164_2019_251]
- Shin, E. J., Dang, D. K., Hwang, Y. G., Tran, H. Q., Sharma, N., Jeong, J. H., Jang, C. G., Nah, S. Y., Nabeshima, T., Yoneda, Y., Cadet, J. L., & Kim, H. C. (2019). Significance of Protein Kinase C in the Neuropsychotoxicity Induced By Methamphetamine-Like Psychostimulants. Neurochemistry International, 124, 162–170. [PubMed] [DOI:10.1016/j.neuint.2019.01.014]
- Karam, C. S., & Javitch, J. A. (2018). Phosphorylation of the Amino Terminus of the Dopamine Transporter: Regulatory Mechanisms and Implications for Amphetamine Action. In Pasternak, G. W., & Coyle, J. T. (Eds.). Apprentices to Genius: A Tribute to Solomon H. Snyder (Advances in Pharmacology, Volume 82) (pp. 205–234). San Diego: Academic Press. [PubMed] [PubMed Central] [DOI:10.1016/bs.apha.2017.09.002]
- Foster, J. D., & Vaughan, R. A. (2017). Phosphorylation Mechanisms in Dopamine Transporter Regulation. Journal of Chemical Neuroanatomy, 83–84, 10–18. [PubMed] [PubMed Central] [DOI:10.1016/j.jchemneu.2016.10.004]
- Vaughan, R. A., & Foster, J. D. (2013). Mechanisms of Dopamine Transporter Regulation in Normal and Disease States. Trends in Pharmacological Sciences, 34(9), 489–496. [PubMed] [PubMed Central] [DOI:10.1016/j.tips.2013.07.005]
- Leviel, V. (2011). Dopamine Release Mediated By the Dopamine Transporter, Facts and Consequences. Journal of Neurochemistry, *118*(4), 475–489. [PubMed] [DOI:10.1111/j.1471-4159.2011.07335.x]
- Schmitt, K. C., & Reith, M. E. (2010). Regulation of the Dopamine Transporter: Aspects Relevant to Psychostimulant Drugs of Abuse. Annals of the New York Academy of Sciences, 1187, 316–340. [PubMed] [DOI:10.1111/j.1749-6632.2009.05148.x]
- Sitte, H. H., & Freissmuth, M. (2010). The Reverse Operation of Na(+)/Cl(-)-Coupled Neurotransmitter Transporters—Why Amphetamines Take Two to Tango. Journal of Neurochemistry, 112(2), 340–355. [PubMed] [PubMed Central] [DOI:10.1111/j.1471-4159.2009.06474.x]
- Eriksen, J., Jørgensen, T. N., & Gether, U. (2010). Regulation of Dopamine Transporter Function By Protein–Protein Interactions: New Discoveries and Methodological Challenges. Journal of Neurochemistry, 113(1), 27–41. [PubMed] [DOI:10.1111/j.1471-4159.2010.06599.x]
The query didn't retrieve any of the relevant Sulzer reviews, but they're as follows:
- Sulzer, D., Sonders, M. S., Poulsen, N. W., & Galli, A. (2005). Mechanisms of Neurotransmitter Release By Amphetamines: A Review. Progress in Neurobiology, 75(6), 406–433. [PubMed] [DOI:10.1016/j.pneurobio.2005.04.003]
- Sulzer, D. (2011). How Addictive Drugs Disrupt Presynaptic Dopamine Neurotransmission. Neuron, 69(4), 628–649. [PubMed] [PubMed Central] [DOI:10.1016/j.neuron.2011.02.010]
- Sulzer, D., Cragg, S. J., & Rice, M. E. (2016). Striatal Dopamine Neurotransmission: Regulation of Release and Uptake. Basal Ganglia, 6(3), 123–148. [PubMed] [PubMed Central] [DOI:10.1016/j.baga.2016.02.001]
I definitely don't want you to read all of the above publications! I haven't read any of them in full myself. I just jumped around and read short key/relevant passages in each one. Of the reviews, I think Reith & Gnegy (2020)[48] is among the best and most applicable. It's the only one I'd recommend definitely reading. Besides that review, if you wanted to, you could just jump around and look at key passages in others like what I did. I think most notably and importantly the parts on amphetamines and PKC. But Reith & Gnegy (2020) on its own covers that pretty well.
From my own reading, many of the reviews state that the mechanisms by which amphetamine(s) activate PKC are unknown. Several of them highlight increased intracellular calcium however. Schmitt & Reith (2010) states that this may be due to amphetamine transport by DAT, co-transport of sodium with amphetamine by DAT, and consequent opening of sodium/calcium antiporters resulting in increased cytosolic calcium.[86] However, this hypothesis seems speculative and unconfirmed. Of the reviews, Shin et al. (2019),[87] Leviel (2011),[88] and Schmitt & Reith (2010)[86] (3 of ~12 reviews) mention or implicate TAAR1 agonism as a possible mechanism of amphetamine-induced PKC activation and MAT efflux (excerpts in the preceding ref cites). Strangely however, Reith no longer mentions TAAR1 in his subsequent 2020 review (Reith & Gnegy, 2020).[48]
In our emails, Miller expressed disappointment to me that many other researchers don't cite his work. He said that he doesn't know why this is. I suspect that there was some enthusiasm early on for TAAR1 involvement in amphetamine MRA actions due to his lab's work. But then that enthusiasm was tempered or faded due to subsequent conflicting research. For instance, other groups being unable to replicate or support his findings, the in-vivo TAAR1 KO mice studies, findings with novel TAAR1 ligands, and so on. I really don't know what's going on there re: Miller's results. But yeah.
I really appreciate your willingness to engage and compromise by the way. – AlyInWikiWonderland (talk, contribs) 05:35, 21 December 2024 (UTC)
Seppi's response to a few comments
| ||
|---|---|---|
|
I'll read one or two tonight and another two tomorrow. To keep this talk page at least somewhat navigable, I'm collapsing my entire response to a few points.
Yes, I'm aware that they didn't use amphetamine. Also, it wasn't MY extrapolation, and it also isn't much of one to begin with given that the only differences are the addition and removal of a single methyl group on the extrapolated compound's backbone; it's kind of like a squeeze theorem: if PEA does something and MA does the same thing, and given that amphetamine contains PEA and MA contains amphetamine, it's fairly likely that they have a common drug effect based on SAR. And yes, I did say SAR only goes so far, but I meant that in terms of the pharmacology of entire structural classes of drugs like substituted amphetamines, and particularly for compounds that have tons of crap tacked onto the base compound's structural backbone. Nonetheless, there are plenty of reviews out there that include analogous diagrams to the one I produced, even if mine preceded them. E.g., https://europepmc.org/article/med/35341572#free-full-text & https://www.cell.com/trends/neurosciences/fulltext/S0166-2236%2822%2900211-9 and FWIW, I never included the plasmalemmal TAAR1-D2sh heterodimer-mediated beta-arrestin 2 signaling pathway in mine or plasmalemmal TAAR1->GIRK pathway. In any event, I just noticed one of the two reviews I linked in this paragraph implicates ERK in TAAR1's signal transduction mechanisms. I'll need to read more on that because that's the first I've heard of that. Also, I am well aware of Sulzer. He low-key came off like a crackpot to me when I read some of his reviews. I don't think I'd want to read another unless he actually says something groundbreaking with evidence to support it. I don't even remember what his theory was; I just remember that I thought it was absurd. Lastly, I still stand behind my assertion that the simplest way to conclude this issue is to buy a selective hTAAR1 full agonist and tetrabenazine from sigma aldrich and just take both; the only problem with doing that is the hTAAR1 agonist needs to be orally bioavailable, BBB-permeable and an hDAT substrate to even reach the cytosol of a dopamine neuron. Not sure any of those exist yet, but I wouldn't mind doing that self-experiment if/when one does, lol. Also, it'd probably cost a few thousand USD, but whatever. I'm sure you know what a dopamine-releasing agent feels like, so there'd be no need to drill holes in anyone's head and probe their dopamine neurons to determine whether it's consistent with the model or not. Seppi333 (Insert 2¢) 05:18, 22 December 2024 (UTC) |
- "
the correct way to address it IMO is to indicate that it's all based on in vitro evidence from animals, cell lines, and human brain tissue, not humans in vivo
"
- "
- At the time of my last reply, I was pretty ambivalent about how this dispute should be resolved. But, I agree with this suggestion and believe it should be implemented alongside both the addition of the table that covers kinase signalling cascades (and their upstream target) and an update amphetamine DA pharmacodynamics diagram to let CaMKII-α share the spotlight with TAAR1. I think that's fair given that CaMKII-α probably accounts for 50% of amphetamine DA efflux. Don't the addiction and FOSB#DeltaFosB articles follow a similar convention as well Re: ΔFosB? The wording doesn't render as the following on the current revision, but I vaguely remember reading something along the lines of:
- "
Based on preclinical evidence involving gene transfer of ΔFosB and ΔJunD in lab animals and evidence from autopsies performed on deceased human cocaine addicts, ΔFosB appears to expression-dependently mediate the development and maintanence of addictions in a subset of neurons in the nucleus accumbens.
"
- "
- I might just be mistaking what I read on those articles back in the day with Nestler's 2013 paper, though. In any event, as is the case with TAAR1, ΔFosB content on wikipedia isn't referenced from papers that discuss in vivo evidence because that would require a brain biopsy; I don't think anyone would be first line to sign up as a participant for such a study given the functional consequences of such a procedure, ignoring the ethics approval process. In any event, here's how I would synthesise an analogous sentence or two in the middle of the second paragraph in amphetamine#pharmacodynamics:
Pharmacodynamic 2nd paragraph synthesis
| ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Edit: I've just realised Amphetamine#Dopamine covers a lot of this evidence too and because this table only covers DAT, maybe it's best to place the wikitable below the first paragraph and above the second paragraph covering VMAT2 in amphetamine#Dopamine (see User:Professional_Crastination/sandbox#Dopamine)? I feel like it might fuck up the viewability of the page too if it's near the top of amphetamine#Pharmacodynamics given how close it'll be to the amphetamine pharmacodynamics image template in the source code. | ||||||||||||||||||||||||||||||||||||||||||
- Also happy to consider modifications to the language used in that synthesis as it was assembled pretty quickly. Any changes that were made are coloured turquoise.
- Re: "
That would likely be because they didn't study that and presumably don't want to hypothesize about.
"
- Re: "
- That makes sense as a potential explanation for the omission. Going back to the ΔFosB example, I couldn't tell you how many literature reviews I've read that discuss mechanisms of addiction sans transcriptional activity involving ΔFosB (well, a lot of the time they're discussing "substance use disorders" which muddies the water). I'm going to leave that at there though because I'm starting to sail into proof by example territory. That said, I'm sure you can appreciate how a number of review articles covering addiction seemingly suck at nuance Re: biomolecular mechanisms.
- Happy holidays! Professional Crastination (talk) 06:29, 25 December 2024 (UTC)
References
[edit]References
|
|---|
|
References
|
Discussion to rename article title from Niacin to Nicotinic acid
[edit]This is an invitation to join the discussion at Talk:Niacin#Requested move 15 December 2024
Thanks! -- Arthurfragoso (talk) 00:42, 16 December 2024 (UTC)
Looking for Research on Turkesterone Efficacy
[edit]Greetings everyone, I recently visited Turkesterone and noticed the page is only a stub. I would like to expand it, particularly in regards to the compound's ability to enhance hypertrophy. I am unsure about the latest verdict on this as I have found articles both stating that it is "extremely" effective as well as completely ineffective.The use of this compound as a supplement was a "trend" amongst bodybuilders around 2021 and is still being pushed by figures such as Greg Doucette (IFBB pro). I think it's important for this topic to be covered and would appreciate any insight on the latest research or anyone providing articles that could be useful (especially if they are reviews). HC226 (talk) 17:23, 27 December 2024 (UTC)