User:Pandemics/2009 flu pandemic
| Pandemic H1N1/09 Influenza | |
|---|---|
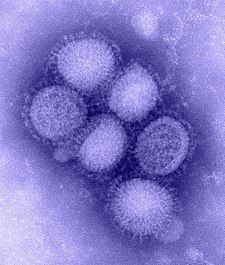 | |
| Electron microscope image of the reassorted H1N1 influenza virus. The viruses are ~100 nanometres in diameter.[1] | |
| Specialty | Infectious disease, pulmonology |
| Influenza (flu) |
|---|
 |
The 2009 flu pandemic or swine flu was an influenza pandemic that lasted from early 2009 to late 2010, and the second of the two pandemics involving H1N1 influenza virus (the first of them being the 1918–1920 Spanish flu pandemic), albeit in a new version. First described in April 2009, the virus appeared to be a new strain of H1N1 which resulted when a previous triple reassortment of bird, swine and human flu viruses further combined with a Eurasian pig flu virus,[2] leading to the term "swine flu".[3] It is estimated that 11–21% of the global population contracted the illness, and 151,000–579,000 died [4].
Unlike most strains of influenza, H1N1 does not disproportionately infect adults older than 60 years; this was an unusual and characteristic feature of the H1N1 pandemic.[5] Even in the case of previously very healthy people, a small percentage will develop pneumonia or acute respiratory distress syndrome (ARDS). This manifests itself as increased breathing difficulty and typically occurs three to six days after initial onset of flu symptoms.[6][7] The pneumonia caused by flu can be either direct viral pneumonia or a secondary bacterial pneumonia. In fact, a November 2009 New England Journal of Medicine article recommended that flu patients whose chest X-ray indicates pneumonia receive both antivirals and antibiotics.[8] In particular, it is a warning sign if a child (and presumably an adult) seems to be getting better and then relapses with high fever, as this relapse may be bacterial pneumonia.[9]
History
[edit]Initially called an "outbreak", widespread H1N1 infection was first recognized in the state of Veracruz, Mexico, with evidence that the virus had been present for months before it was officially called an "epidemic".[10] The Mexican government closed most of Mexico City's public and private facilities in an attempt to contain the spread of the virus; however, it continued to spread globally, and clinics in some areas were overwhelmed by infected people. In late April the World Health Organization (WHO) declared its first ever "public health emergency of international concern," or PHEIC,[11] and in June, the WHO and the U.S. CDC stopped counting cases and declared the outbreak a pandemic.[12]
Despite being informally called "swine flu", the H1N1 flu virus cannot be spread by eating pork or pork products;[13][14] similar to other influenza viruses, it is typically contracted by person to person transmission through respiratory droplets.[15] Symptoms usually last 4–6 days.[16] Antivirals (oseltamivir or zanamivir) were recommended for those with more severe symptoms or those in an at-risk group.[17]
The pandemic began to taper off in November 2009,[18] and by May 2010, the number of cases was in steep decline.[19][20][21][22] On 10 August 2010, the Director-General of the WHO, Margaret Chan, announced the end of the H1N1 pandemic,[23] and announced that the H1N1 influenza event has moved into the post-pandemic period.[24] According to the latest WHO statistics (as of July 2010), the virus has killed more than 18,000 people since it appeared in April 2009, however they state that the total mortality (including deaths unconfirmed or unreported) from the H1N1 strain is "unquestionably higher".[19][25] Critics claimed the WHO had exaggerated the danger, spreading "fear and confusion" rather than "immediate information".[26] The WHO began an investigation to determine[27] whether it had "frightened people unnecessarily".[28] A flu follow-up study done in September 2010, found that "the risk of most serious complications was not elevated in adults or children."[29] In a 5 August 2011 PLoS ONE article, researchers estimated that the 2009 H1N1 global infection rate was 11% to 21%, lower than what was previously expected.[30] However, by 2012, research showed that as many as 579,000 people could have been killed by the disease, as only those fatalities confirmed by laboratory testing were included in the original number, and meant that many of those without access to health facilities went uncounted. The majority of these deaths occurred in Africa and Southeast Asia. Experts, including the WHO, have agreed that an estimated 284,500 people were killed by the disease, much higher than the initial death toll.[31][32]
Classification
[edit]The initial outbreak was called the "H1N1 influenza", or "Swine Flu" by American media. It is called the pandemic H1N1/09 virus by the WHO,[33] while the U.S. Centers for Disease Control and Prevention refer to it as "novel influenza A (H1N1)" or "2009 H1N1 flu".[34] In the Netherlands, it was originally called "Pig Flu", but is now called "New Influenza A (H1N1)" by the national health institute, although the media and general population use the name "Mexican Flu". South Korea and Israel briefly considered calling it the "Mexican virus".[35] Later, the South Korean press used "SI", short for "swine influenza". Taiwan suggested the names "H1N1 flu" or "new flu", which most local media adopted.[36] The World Organization for Animal Health proposed the name "North American influenza".[37] The European Commission adopted the term "novel flu virus".[38]
Signs and symptoms
[edit]The symptoms of H1N1 flu are similar to those of other influenzas, and may include fever, cough (typically a "dry cough"), headache, muscle or joint pain, sore throat, chills, fatigue, and runny nose. Diarrhea, vomiting, and neurological problems have also been reported in some cases.[39][40] People at higher risk of serious complications include those aged over 65, children younger than 5, children with neurodevelopmental conditions, pregnant women (especially during the third trimester),[6][41] and those of any age with underlying medical conditions, such as asthma, diabetes, obesity, heart disease, or a weakened immune system (e.g., taking immunosuppressive medications or infected with HIV).[42] More than 70% of hospitalizations in the U.S. have been people with such underlying conditions, according to the CDC.[43]
In September 2009, the CDC reported that the H1N1 flu "seems to be taking a heavier toll among chronically ill children than the seasonal flu usually does."[9] Through 8 August 2009, the CDC had received 36 reports of paediatric deaths with associated influenza symptoms and laboratory-confirmed pandemic H1N1 from state and local health authorities within the United States, with 22 of these children having neurodevelopmental conditions such as cerebral palsy, muscular dystrophy, or developmental delays.[44] "Children with nerve and muscle problems may be at especially high risk for complications because they cannot cough hard enough to clear their airways".[9] From 26 April 2009, to 13 February 2010, the CDC had received reports of the deaths of 277 children with laboratory-confirmed 2009 influenza A (H1N1) within the United States.[45]
Severe cases
[edit]The World Health Organization reports that the clinical picture in severe cases is strikingly different from the disease pattern seen during epidemics of seasonal influenza. While people with certain underlying medical conditions are known to be at increased risk, many severe cases occur in previously healthy people. In severe cases, patients generally begin to deteriorate around three to five days after symptom onset. Deterioration is rapid, with many patients progressing to respiratory failure within 24 hours, requiring immediate admission to an intensive care unit. Upon admission, most patients need immediate respiratory support with mechanical ventilation.[46]
Complications
[edit]Most complications have occurred among previously healthy individuals, with obesity and respiratory disease as the strongest risk factors. Pulmonary complications are common. Primary influenza pneumonia occurs most commonly in adults and may progress rapidly to acute lung injury requiring mechanical ventilation. Secondary bacterial infection is more common in children. Staphylococcus aureus, including methicillin-resistant strains, is an important cause of secondary bacterial pneumonia with a high mortality rate; streptococcus pneumoniae is the second most important cause of secondary bacterial pneumonia for children and primary for adults. Neuromuscular and cardiac complications are unusual but may occur.[47]
A United Kingdom investigation of risk factors for hospitalisation and poor outcome with pandemic A/H1N1 influenza looked at 631 patients from 55 hospitals admitted with confirmed infection from May through September 2009. 13% were admitted to a high dependency or intensive care unit and 5% died; 36% were aged <16 years and 5% were aged ≥65 years. Non-white and pregnant patients were over-represented. 45% of patients had at least one underlying condition, mainly asthma, and 13% received antiviral drugs before admission. Of 349 with documented chest x-rays on admission, 29% had evidence of pneumonia, but bacterial co-infection was uncommon. Multivariate analyses showed that physician-recorded obesity on admission and pulmonary conditions other than asthma or chronic obstructive pulmonary disease (COPD) were associated with a severe outcome, as were radiologically confirmed pneumonia and a raised C-reactive protein (CRP) level (≥100 mg/l). 59% of all in-hospital deaths occurred in previously healthy people.[48]
Fulminant (sudden-onset) myocarditis has been linked to infection with H1N1, with at least four cases of myocarditis confirmed in patients also infected with A/H1N1. Three out of the four cases of H1N1-associated myocarditis were classified as fulminant, and one of the patients died.[49] Also, there appears to be a link between severe A/H1N1 influenza infection and pulmonary embolism. In one report, five out of 14 patients admitted to the intensive care unit with severe A/H1N1 infection were found to have pulmonary emboli.[50]
An article published in JAMA in September 2010[51] challenged previous reports and stated that children infected in the 2009 flu pandemic were no more likely to be hospitalised with complications or get pneumonia than those who catch seasonal strains. Researchers found that about 1.5% of children with the H1N1 swine flu strain were hospitalised within 30 days, compared with 3.7% of those sick with a seasonal strain of H1N1 and 3.1% with an H3N2 virus.[29]
Diagnosis
[edit]Confirmed diagnosis of pandemic H1N1 flu requires testing of a nasopharyngeal, nasal or oropharyngeal tissue swab from the patient.[52] Real-time RT-PCR is the recommended test as others are unable to differentiate between pandemic H1N1 and regular seasonal flu.[52] However, most people with flu symptoms do not need a test for pandemic H1N1 flu specifically, because the test results usually do not affect the recommended course of treatment.[53] The U.S. CDC recommend testing only for people who are hospitalized with suspected flu, pregnant women and people with weakened immune systems.[53] For the mere diagnosis of influenza and not pandemic H1N1 flu specifically, more widely available tests include rapid influenza diagnostic tests (RIDT), which yield results in about 30 minutes, and direct and indirect immunofluorescence assays (DFA and IFA), which take 2–4 hours.[54] Due to the high rate of RIDT false negatives, the CDC advises that patients with illnesses compatible with novel influenza A (H1N1) virus infection but with negative RIDT results should be treated empirically based on the level of clinical suspicion, underlying medical conditions, severity of illness and risk for complications, and if a more definitive determination of infection with influenza virus is required, testing with rRT-PCR or virus isolation should be performed.[55] Rhonda Medows of the Georgia Department of Community Health states that the rapid tests are incorrect anywhere from 30% to 90% of the time and warns doctors in her state not to use them because they are wrong so often.[56] The use of RIDTs has also been questioned by researcher Paul Schreckenberger of the Loyola University Health System, who suggests that rapid tests may actually pose a dangerous public health risk.[57] Nikki Shindo of the WHO has expressed regret at reports of treatment being delayed by waiting for H1N1 test results and suggests, "[D]octors should not wait for the laboratory confirmation but make diagnosis based on clinical and epidemiological backgrounds and start treatment early".[58]
On 22 June 2010, the CDC announced a new test called the "CDC Influenza 2009 A (H1N1)pdm Real-Time RT-PCR Panel (IVD)". It uses a molecular biology technique to detect influenza A viruses and specifically the 2009 H1N1 virus. The new test will replace the previous real-time RT-PCR diagnostic test used during the 2009 H1N1 pandemic, which received an emergency use authorization from the U.S. Food and Drug Administration in April 2009. Tests results are available in four hours and are 96% accurate.[59]
Cause
[edit]The virus was found to be a novel strain of influenza for which extant vaccines against seasonal flu provided little protection. A study at the U.S. Centers for Disease Control and Prevention published in May 2009 found that children had no preexisting immunity to the new strain but that adults, particularly those older than 60, had some degree of immunity. Children showed no cross-reactive antibody reaction to the new strain, adults aged 18 to 60 had 6–9%, and older adults 33%.[60][61] While it has been thought that these findings suggest the partial immunity in older adults may be due to previous exposure to similar seasonal influenza viruses, a November 2009 study of a rural unvaccinated population in China found only a 0.3% cross-reactive antibody reaction to the H1N1 strain, suggesting that previous vaccinations for seasonal flu and not exposure may have resulted in the immunity found in the older U.S. population.[62]
Analyses of the genetic sequences of the first isolates, promptly shared on the GISAID database according to Nature and WHO,[63][64] soon determined that the strain contains genes from five different flu viruses: North American swine influenza, North American avian influenza, human influenza and two swine influenza viruses typically found in Asia and Europe. Further analysis has shown that several proteins of the virus are most similar to strains that cause mild symptoms in humans, leading virologist Wendy Barclay to suggest on 1 May 2009, that the initial indications are that the virus was unlikely to cause severe symptoms for most people.[65]
The virus is currently less lethal than previous pandemic strains and kills about 0.01–0.03% of those infected; the 1918 influenza was about one hundred times more lethal and had a case fatality rate of 2–3%.[66] By 14 November 2009, the virus had infected one in six Americans with 200,000 hospitalisations and 10,000 deaths – as many hospitalizations and fewer deaths than in an average flu season overall, but with much higher risk for those under 50. With deaths of 1,100 children and 7,500 adults 18 to 64, these figures "are much higher than in a usual flu season".[67]
In June 2010, scientists from Hong Kong reported discovery of a new swine flu virus which is a hybrid of the pandemic H1N1 virus and viruses previously found in pigs. It is the first report of a reassortment of the pandemic virus, which in humans has been slow to evolve. Nancy Cox, head of the influenza division at the U.S. Centers for Disease Control and Prevention, has said, "This particular paper is extremely interesting because it demonstrates for the first time what we had worried about at the very onset of the pandemic, and that is that this particular virus, when introduced into pigs, could reassort with the resident viruses in pigs and we would have new gene constellations. And bingo, here we are." Pigs have been termed the mixing vessel of flu because they can be infected both by avian flu viruses, which rarely directly infect people, and by human viruses. When pigs become simultaneously infected with more than one virus, the viruses can swap genes, producing new variants which can pass to humans and sometimes spread amongst them.[68] "Unlike the situation with birds and humans, we have a situation with pigs and humans where there's a two-way street of exchange of viruses. With pigs it's very much a two-way street".[69]
Transmission
[edit]Spread of the H1N1 virus is thought to occur in the same way that seasonal flu spreads. Flu viruses are spread mainly from person to person through coughing or sneezing by people with influenza. Sometimes people may become infected by touching something – such as a surface or object – with flu viruses on it and then touching their face. "Avoid touching your eyes, nose or mouth. Germs spread this way".[13]
The basic reproduction number (the average number of other individuals whom each infected individual will infect, in a population which has no immunity to the disease) for the 2009 novel H1N1 is estimated to be 1.75.[70] A December 2009 study found that the transmissibility of the H1N1 influenza virus in households is lower than that seen in past pandemics. Most transmissions occur soon before or after the onset of symptoms.[71]
The H1N1 virus has been transmitted to animals, including swine, turkeys, ferrets, household cats, at least one dog and a cheetah.[72][73][74][75]
Prevention
[edit]The H1N1 vaccine was initially in short supply and in the U.S., the CDC recommended that initial doses should go to priority groups such as pregnant women, people who live with or care for babies under six months old, children six months to four years old and health-care workers.[76] In the UK, the NHS recommended vaccine priority go to people over six months old who were clinically at risk for seasonal flu, pregnant women and households of people with compromised immunity.[77]
Although it was initially thought that two injections would be required, clinical trials showed that the new vaccine protected adults "with only one dose instead of two", and so the limited vaccine supplies would go twice as far as had been predicted.[78][79] Health officials worldwide were also concerned because the virus was new and could easily mutate and become more virulent, even though most flu symptoms were mild and lasted only a few days without treatment. Officials also urged communities, businesses and individuals to make contingency plans for possible school closures, multiple employee absences for illness, surges of patients in hospitals and other effects of potentially widespread outbreaks.[80] Disaster response organizations such as Direct Relief helped by providing protective items to clinical workers to help them stay healthy throughout flu season.[81][82]
In February 2010, the CDC's Advisory Committee on Immunization Practices voted for "universal" flu vaccination in the U.S. to include all people over six months of age. The 2010–2011 vaccine will protect against the 2009 H1N1 pandemic virus and two other flu viruses.[83]
Public health response
[edit]
On 27 April 2009, the European Union health commissioner advised Europeans to postpone nonessential travel to the United States or Mexico. This followed the discovery of the first confirmed case in Spain.[84] On 6 May 2009, the Public Health Agency of Canada announced that their National Microbiology Laboratory (NML) had mapped the genetic code of the swine flu virus, the first time that had been done.[85] In the U.K., the National Health Service launched a website, the National Pandemic Flu Service,[86] allowing patients to self-assess and get an authorisation number for antiviral medication. The system was expected to reduce the burden on general practitioners.[77]
U.S. officials observed that six years of concern about H5N1 avian flu did much to prepare for the current H1N1 flu outbreak, noting that after H5N1 emerged in Asia, ultimately killing about 60% of the few hundred people infected by it over the years, many countries took steps to try to prevent any similar crisis from spreading further.[87] The CDC and other U.S. governmental agencies[88] used the summer lull to take stock of the United States' response to H1N1 flu and attempt to patch any gaps in the public health safety net before flu season started in early autumn.[89] Preparations included planning a second influenza vaccination program in addition to that for seasonal influenza, and improving coordination between federal, state and local governments and private health providers.[89] On 24 October 2009, U.S. President Obama declared swine flu a national emergency, giving Secretary of Health and Human Services Kathleen Sebelius authority to grant waivers to requesting hospitals from usual federal requirements.[90]
Vaccines
[edit]
By 19 November 2009, doses of vaccine had been administered in over 16 countries. A 2009 review by the U.S. National Institutes of Health (NIH) concluded that the 2009 H1N1 vaccine has a safety profile similar to that of seasonal vaccine.
In 2011, a study from the US Flu Vaccine Effectiveness Network estimated the overall effectiveness of all pandemic H1N1 vaccines at 56%. A CDC study released 28 January 2013, estimated that the Pandemic H1N1 vaccine saved roughly 300 lives and prevented about 1 million illnesses in the US. The study concluded that had the vaccination program started 2 weeks earlier, close to 60% more cases could have been prevented. The study was based on an effectiveness in preventing cases, hospitalizations, and deaths of 62% for all subgroups except people over 65, for whom the effectiveness was estimated at 43%. The effectiveness was based on European and Asian studies and expert opinion.[3] The delay in vaccine administration demonstrated the shortcomings of the world's capacity for vaccine-production, as well as problems with international distribution. Some manufacturers and wealthy countries had concerns regarding liability and regulations, as well as the logistics of transporting, storing, and administering vaccines to be donated to poorer countries.[91]
Accusations of conflict of interest
[edit]In January 2010, Wolfgang Wodarg, a German deputy who trained as a physician and now chairs the health committee at the Council of Europe, claimed major firms had organised a "campaign of panic" to put pressure on the World Health Organization (WHO) to declare a "false pandemic" to sell vaccines. Wodarg said the WHO's "false pandemic" flu campaign is "one of the greatest medicine scandals of the century". He said that the "false pandemic" campaign began in May 2009 in Mexico City, when a hundred or so "normal" reported influenza cases were declared to be the beginning of a threatening new pandemic, although he said there was little scientific evidence for this. Nevertheless, he argued that the WHO, "in cooperation with some big pharmaceutical companies and their scientists, re-defined pandemics", removing the statement that "an enormous amount of people have contracted the illness or died" from its existing definition and replacing it by stating simply that there has to be a virus, spreading beyond borders and to which people have no immunity.[92]
The WHO responded by stating that they take their duty to provide independent advice seriously and guarded against interference from outside interests. Announcing a review of the WHO's actions, spokeswoman Fadela Chaib stated: "Criticism is part of an outbreak cycle. We expect and indeed welcome criticism and the chance to discuss it".[93][94] In March 2010, the Council of Europe launched an enquiry into "the influence of the pharmaceutical companies on the global swine flu campaign", and a preliminary report is in preparation.[95]
On 12 April 2010, Keiji Fukuda, the WHO's top influenza expert, stated that the system leading to the declaration of a pandemic led to confusion about H1N1 circulating around the world, and he expressed concern that there was a failure to communicate in regard to uncertainties about the new virus, which turned out to be not as deadly as feared. WHO Director-General Margaret Chan has appointed 29 flu experts from outside the organization to conduct a review of WHO's handling of the H1N1 flu pandemic. She has told them, "We want a frank, critical, transparent, credible and independent review of our performance".[96]
In June 2010, Fiona Godlee, editor-in-chief of the BMJ, published an editorial which criticised the WHO, saying that an investigation had disclosed that some of the experts advising WHO on the pandemic had financial ties with drug companies which were producing antivirals and vaccines.[97] Margaret Chan, Director-General of the WHO, replied stating, "Without question, the BMJ feature and editorial will leave many readers with the impression that WHO's decision to declare a pandemic was at least partially influenced by a desire to boost the profits of the pharmaceutical industry. The bottom line, however, is that decisions to raise the level of pandemic alert were based on clearly defined virological and epidemiological criteria. It is hard to bend these criteria, no matter what the motive".[96]
Infection control
[edit]Travel precautions
[edit]

On 7 May 2009, the WHO stated that containment was not feasible and that countries should focus on mitigating the effect of the virus. They did not recommend closing borders or restricting travel.[98] On 26 April 2009, the Chinese government announced that visitors returning from flu-affected areas who experienced flu-like symptoms within two weeks would be quarantined.[99]
U.S. airlines had made no major changes as of the beginning of June 2009, but continued standing practices which include looking for passengers with symptoms of flu, measles or other infections, and relying on in-flight air filters to ensure that aircraft were sanitised.[100] Masks were not generally provided by airlines and the CDC did not recommend that airline crews wear them.[100] Some non-U.S. airlines, mostly Asian, including Singapore Airlines, China Eastern Airlines, China Southern Airlines, Cathay Pacific and Aeromexico, took measures such as stepping up cabin cleaning, installing state-of-the-art air filters and allowing in-flight staff to wear face masks.[100]
According to studies conducted in Australia and Japan, screening individuals for influenza symptoms at airports during the 2009 H1N1 outbreak was not an effective method of infection control.[101][102]
Schools
[edit]U.S. government officials have been especially concerned about schools because the H1N1 flu virus appears to disproportionately affect young and school-age people, between six months and 24 years of age.[103] The H1N1 outbreak led to numerous precautionary school closures in some areas. Rather than closing schools, the CDC recommended that students and school workers with flu symptoms should stay home for either seven days total, or until 24 hours after symptoms subsided, whichever was longer.[104] The CDC also recommended that colleges should consider suspending fall 2009 classes if the virus began to cause severe illness in a significantly larger share of students than the previous spring. They also urged schools to suspend rules, such as penalties for late papers or missed classes or requirements for a doctor's note, to enforce "self-isolation" and prevent students from venturing out while ill;[105] schools were advised to set aside a room for people developing flu-like symptoms while they waited to go home and to have ill students or staff and those caring for them use face masks.[106]
In California, school districts and universities were on alert and worked with health officials to launch education campaigns. Many planned to stockpile medical supplies and discuss worst-case scenarios, including plans to provide lessons and meals for low-income children in case elementary and secondary schools closed.[107] University of California campuses stockpiled supplies, from paper masks and hand sanitizer to food and water.[107] To help prepare for contingencies, University of Maryland School of Medicine professor of pediatrics James C. King Jr. suggested that every county should create an "influenza action team" to be run by the local health department, parents and school administrators.[108] By 28 October 2009, about 600 schools in the United States had been temporarily closed, affecting over 126,000 students in 19 states.[109]
Workplace
[edit]Fearing a worst-case scenario, the U.S. Department of Health and Human Services (HHS), the Centers for Disease Control and Prevention and the Department of Homeland Security (DHS) developed updated guidance[110] and a video for employers to use as they developed plans to respond to the H1N1 outbreak. The guidance suggested that employers consider and communicate their objectives, such as reducing transmission among staff, protecting people who are at increased risk of influenza-related complications from becoming infected, maintaining business operations, and minimising adverse effects on other entities in their supply chains.[110]
The CDC estimated that as much as 40% of the workforce might be unable to work at the peak of the pandemic due to the need for many healthy adults to stay home and care for an ill family member,[111] and advised that individuals should have steps in place should a workplace close down or a situation arise that requires working from home.[112] The CDC further advised that persons in the workplace should stay home sick for seven days after getting the flu, or 24 hours after symptoms end, whichever is longer.[104]
In the UK, the Health and Safety Executive (HSE) also issued general guidance for employers.[113]
Facial masks
[edit]
The U.S. CDC does not recommend use of face masks or respirators in non-health care settings, such as schools, workplaces, or public places, with a few exceptions: people who are ill with the virus when around other people, and people who are at risk for severe illness while caring for someone with the flu.[114] There has been some disagreement about the value of wearing facial masks, some experts fearing that masks may give people a false sense of security and should not replace other standard precautions.[115] Masks may benefit people in close contact with infected persons, but it is unknown whether they prevent H1N1 flu infection.[115] Yukihiro Nishiyama, professor of virology at Nagoya University's School of Medicine, commented that the masks are "better than nothing, but it's hard to completely block out an airborne virus since it can easily slip through the gaps".[116]
According to mask manufacturer 3M, masks will filter out particles in industrial settings, but "there are no established exposure limits for biological agents such as swine flu virus".[115] However, despite the lack of evidence of effectiveness, the use of such masks is common in Asia.[116][117] They are particularly popular in Japan, where cleanliness and hygiene are highly valued and where etiquette obligates those who are sick to wear masks to avoid spreading disease.[116]
Quarantine
[edit]During the height of the fear of a pandemic, some countries initiated or threatened to initiate quarantines of foreign visitors suspected of having or being in contact with others who may have been infected. In May 2009, the Chinese government confined 21 U.S. students and three teachers to their hotel rooms.[118] As a result, the US State Department issued a travel alert about China's anti-flu measures and warned travellers against travelling to China if ill.[119] In Hong Kong, an entire hotel was quarantined with 240 guests;[120] Australia ordered a cruise ship with 2,000 passengers to stay at sea because of a swine flu threat.[121] Egyptian Muslims who went on the annual pilgrimage to Mecca risked being quarantined upon their return.[122] Russia and Taiwan said they would quarantine visitors with fevers who come from areas where the flu was present.[123] Japan quarantined 47 airline passengers in a hotel for a week in mid-May,[124] then in mid-June India suggested pre-screening "outbound" passengers from countries thought to have a high rate of infection.[125]
Pigs and food safety
[edit]The pandemic virus is a type of swine influenza, derived originally from a strain which lived in pigs, and this origin gave rise to the common name of "swine flu". This term is widely used by mass media. The virus has been found in American hogs,[126] and Canadian[127] as well as in hogs in Northern Ireland, Argentina, and Norway.[128] Leading health agencies and the United States Secretary of Agriculture have stressed that eating properly cooked pork or other food products derived from pigs will not cause flu.[129][130] Nevertheless, on 27 April, Azerbaijan imposed a ban on the importation of animal husbandry products from the entire Americas.[131] The Indonesian government also halted the importation of pigs and initiated the examination of 9 million pigs in Indonesia.[132] The Egyptian government ordered the slaughter of all pigs in Egypt on 29 April 2009.[133]
Treatment
[edit]A number of methods have been recommended to help ease symptoms, including adequate liquid intake and rest.[134] Over-the-counter pain medications such as acetaminophen and ibuprofen do not kill the virus; however, they may be useful to reduce symptoms.[135] Aspirin and other salicylate products should not be used by people under 16 with any flu-type symptoms because of the risk of developing Reye's Syndrome.[136]
If the fever is mild and there are no other complications, fever medication is not recommended.[135] Most people recover without medical attention, although those with pre-existing or underlying medical conditions are more prone to complications and may benefit from further treatments.[137]
People in at-risk groups should be treated with antivirals (oseltamivir or zanamivir) as soon as possible when they first experience flu symptoms. The at-risk groups include pregnant and post partum women, children under two years old, and people with underlying conditions such as respiratory problems.[17] People who are not in an at-risk group who have persistent or rapidly worsening symptoms should also be treated with antivirals. People who have developed pneumonia should be given both antivirals and antibiotics, as in many severe cases of H1N1-caused illness, bacterial infection develops.[58] Antivirals are most useful if given within 48 hours of the start of symptoms and may improve outcomes in hospitalised patients.[138] In those beyond 48 hours who are moderately or severely ill, antivirals may still be beneficial.[15] If oseltamivir (Tamiflu) is unavailable or cannot be used, zanamivir (Relenza) is recommended as a substitute.[17][139] Peramivir is an experimental antiviral drug approved for hospitalised patients in cases where the other available methods of treatment are ineffective or unavailable.[140]
To help avoid shortages of these drugs, the U.S. CDC recommended oseltamivir treatment primarily for people hospitalised with pandemic flu; people at risk of serious flu complications due to underlying medical conditions; and patients at risk of serious flu complications. The CDC warned that the indiscriminate use of antiviral medications to prevent and treat influenza could ease the way for drug-resistant strains to emerge, which would make the fight against the pandemic that much harder. In addition, a British report found that people often failed to complete a full course of the drug or took the medication when not needed.[141]
Side effects
[edit]Both medications have known side effects, including lightheadedness, chills, nausea, vomiting, loss of appetite and trouble breathing. Children were reported to be at increased risk of self-injury and confusion after taking oseltamivir.[134] The WHO warn against buying antiviral medications from online sources, and estimate that half the drugs sold by online pharmacies without a physical address are counterfeit.[142]
Resistance
[edit]In December 2012, 2010, the World Health Organization (WHO) reported 314 samples of the 2009 pandemic H1N1 flu tested worldwide have shown resistance to oseltamivir (Tamiflu).[143] This is not totally unexpected as 99.6% of the seasonal H1N1 flu strains tested have developed resistance to oseltamivir.[144] No circulating flu has yet shown any resistance to zanamivir (Relenza), the other available anti-viral.[145]
Effectiveness of antivirals questioned
[edit]On 8 December 2009, the Cochrane Collaboration, which reviews medical evidence, announced in a review published in BMJ that it had reversed its previous findings that the antiviral drugs oseltamivir (Tamiflu) and zanamivir (Relenza) can ward off pneumonia and other serious conditions linked to influenza. They reported that an analysis of 20 studies showed oseltamivir offered mild benefits for healthy adults if taken within 24 hours of onset of symptoms, but found no clear evidence it prevented lower respiratory tract infections or other complications of influenza.[146][147] Their published finding relates only to its use in healthy adults with influenza; they say nothing about its use in patients judged to be at high risk of complications (pregnant women, children under five and those with underlying medical conditions), and uncertainty over its role in reducing complications in healthy adults may still leave it as a useful drug for reducing the duration of symptoms. The drugs might eventually be demonstrated to be effective against flu-related complications; in general, the Cochrane Collaboration concluded "Paucity of good data".[147][148]
Some specific results from the BMJ article include: "The efficacy of oral oseltamivir against symptomatic laboratory confirmed influenza was 61% (risk ratio 0.39, 95% confidence interval 0.18 to 0.85) at 75 mg daily ... The remaining evidence suggests oseltamivir did not reduce influenza related lower respiratory tract complications (risk ratio 0.55, 95% confidence interval 0.22 to 1.35)".[147] Notice especially the wide range for this second result.
Epidemiology
[edit]{{2009 flu pandemic data}} While it is not known precisely where or when the virus originated,[149][150] analyses in scientific journals have suggested that the H1N1 strain responsible for the 2009 outbreak first evolved in September 2008 and circulated amongst humans for several months before being formally recognised and identified as a novel strain of influenza.[149][151]
Mexico
[edit]The virus was first reported in two U.S. children in March 2009, but health officials have reported that it apparently infected people as early as January 2009 in Mexico.[152] The outbreak was first detected in Mexico City on 18 March 2009;[153] immediately after the outbreak was officially announced, Mexico notified the U.S. and World Health Organization, and within days of the outbreak Mexico City was "effectively shut down".[154] Some countries cancelled flights to Mexico while others halted trade. Calls to close the border to contain the spread were rejected.[154] Mexico already had hundreds of non-lethal cases before the outbreak was officially discovered, and was therefore in the midst of a "silent epidemic". As a result, Mexico was reporting only the most serious cases which showed more severe signs different from those of normal flu, possibly leading to a skewed initial estimate of the case fatality rate.[153]
United States
[edit]The new strain was first identified by the CDC in two children, neither of whom had been in contact with pigs. The first case, from San Diego County, California, was confirmed from clinical specimens (nasopharyngeal swab) examined by the CDC on 14 April 2009. A second case, from nearby Imperial County, California, was confirmed on 17 April. The patient in the first confirmed case had flu symptoms including fever and cough on clinical examination on 30 March, and the second on 28 March.[155]
The first confirmed H1N1/09 pandemic flu death, which occurred at Texas Children's Hospital in Houston, Texas, was of a toddler from Mexico City who was visiting family in Brownsville, Texas, before being air-lifted to Houston for treatment.[156]
Data reporting and accuracy
[edit]Influenza surveillance information "answers the questions of where, when, and what influenza viruses are circulating. Sharing of such information is especially crucial during an emergent pandemic as in April 2009, when the genetic sequences of the initial viruses were rapidly and openly shared via the GISAID Initiative within days of identification,[157] playing a key role in facilitating an early response to the evolving pandemic.[158][159][160] Surveillance is used to determine if influenza activity is increasing or decreasing, but cannot be used to ascertain how many people have become ill with influenza".[161] For example, as of late June 2009, influenza surveillance information showed the U.S. had nearly 28,000 laboratory-confirmed cases including 3,065 hospitalisations and 127 deaths; but mathematical modelling showed an estimated 1 million Americans currently had the 2009 pandemic flu, according to Lyn Finelli, a flu surveillance official with the CDC.[162] Estimating deaths from influenza is also a complicated process. In 2005, influenza only appeared on the death certificates of 1,812 people in the US. The average annual US death toll from flu is, however, estimated to be 36,000.[163] The CDC explains:[164] "[I]nfluenza is infrequently listed on death certificates of people who die from flu-related complications" and hence, "Only counting deaths where influenza was included on a death certificate would be a gross underestimation of influenza's true impact".
Influenza surveillance information on the 2009 H1N1 flu pandemic is available, but almost no studies attempted to estimate the total number of deaths attributable to H1N1 flu. Two studies were carried out by the CDC; the later of them estimated that between 7,070 and 13,930 deaths were attributable to H1N1 flu from April to 14 November 2009.[165] During the same period, 1642 deaths were officially confirmed as caused by H1N1 flu.[166][167] The WHO state that total mortality (including deaths unconfirmed or unreported) from H1N1 flu is "unquestionably higher" than their own confirmed death statistics.[168]
The initial outbreak received a week of near-constant media attention. Epidemiologists cautioned that the number of cases reported in the early days of an outbreak can be very inaccurate and deceptive, due to several causes, among them selection bias, media bias and incorrect reporting by governments. Inaccuracies could also be caused by authorities in different countries looking at differing population groups. Furthermore, countries with poor health care systems and older laboratory facilities may take longer to identify or report cases.[169] "[E]ven in developed countries the [numbers of flu deaths] are uncertain, because medical authorities don't usually verify who actually died of influenza and who died of a flu-like illness".[170] Joseph S. Bresee (the CDC flu division's epidemiology chief) and Michael Osterholm (director of the Center for Infectious Disease Research and Policy) have pointed out that millions of people have had H1N1 flu, usually in a mild form, so the numbers of laboratory-confirmed cases were actually meaningless, and in July 2009, the WHO stopped keeping count of individual cases and focused more on major outbreaks.[171]
Follow-up
[edit]A Wisconsin study published in the Journal of the American Medical Association in September 2010, reported that findings showed that the 2009 H1N1 flu was no more severe than the seasonal flu. "The risk of most serious complications was not elevated in adults or children", the study's authors wrote. "Children were disproportionately affected by 2009 H1N1 infection, but the perceived severity of symptoms and risk of serious outcomes were not increased." Children infected in the 2009 H1N1 flu pandemic were no more likely to be hospitalized with complications or get pneumonia than those who catch seasonal strains. About 1.5% of children with the H1N1 swine flu strain were hospitalized within 30 days, compared with 3.7% of those sick with a seasonal strain of H1N1 and 3.1% with an H3N2 virus.[172]
CDC illness and death estimates from April 2009 to April 2010, in the US are as follows:
- CDC estimates that between 43 million and 89 million cases of 2009 H1N1 occurred between April 2009 and 10 April 2010. The mid-level in this range is about 61 million people infected with 2009 H1N1.
- CDC estimates that between about 195,000 and 403,000 H1N1-related hospitalizations occurred between April 2009 and 10 April 2010. The mid-level in this range is about 274,000 2009 H1N1-related hospitalizations.
- CDC estimates that between about 8,870 and 18,300 2009 H1N1-related deaths occurred between April 2009 and 10 April 2010. The mid-level in this range is about 12,470 2009 H1N1-related deaths.[173][174][175]
It is often stated that about 36,000 die from the seasonal flu in the U.S. each year,[176] and this is frequently understood as an indication that the H1N1 strain was not as severe as seasonal influenza. The 36,000 estimate was presented in a 2003 study by CDC scientists published in the Journal of the American Medical Association but only refers to a period from 1990–91 through 1998–99. During those years, the number of estimated deaths ranged from 17,000 to 52,000, with an average of about 36,000. The JAMA study also looked at seasonal influenza-associated deaths over a 23-year period, from 1976–77 and 1998–99. During that period, estimates of respiratory and circulatory influenza-associated deaths ranged from about 5,000 to about 52,000, with an average of about 25,000. While the 36,000 number is often cited, it's important to note that during that decade, influenza A (H3N2) was the predominant virus during most of the seasons, and H3N2 influenza viruses are typically associated with higher death rates. CDC believes that the range of deaths over the past 31 years (~3,000 to ~49,000) is a more accurate representation of the unpredictability and variability of flu-associated deaths.[177] The annual toll from seasonal influenza in the US is more accurately estimated at 3000–49,000 deaths per year. So the H1N1 pandemic estimated mortality of 8,870 to 18,300, places it in the mid-range of estimates.[178]
The 2009 pandemic caused hospitals around the country to make significant preparations in terms of hospital surge capacities, especially within the emergency department and among vulnerable populations. In many cases, hospitals were relatively successful in making sure that those patients most severely affected by the influenza strain were able to be seen, treated, and discharged in an efficient manner. A proper case-study of the preparation, planning, mitigation, and response efforts during the Fall of 2009 is that of the Children's Hospital of Philadelphia (CHOP). For example, CHOP took several steps to increase the emergency department (ED) surge capacity response abilities through careful planning and mitigation efforts. To increase ED capacity and response, CHOP used portions of the main lobby area as an ED waiting room; several of the region's hospital-based outpatient facilities were in use during evening and weekend hours for non-emergency cases; the ED's 24-hour short-stay unit was utilized to care for ED patients in a longer-term capacity; non-board certified physicians (in pediatric emergency medicine) and inpatient-unit medical nurses were utilized for ED patient care; hospital units normally utilized for other medical or therapeutic purposes were transformed into ED patient rooms; and rooms normally used for only one patient were expanded to at least a capacity of 2[179]
Comparisons to other pandemics and epidemics
[edit]Annual influenza epidemics are estimated to affect 5–15% of the global population. Although most cases are mild, these epidemics still cause severe illness in 3–5 million people and 290,000–650,000 deaths worldwide.[180] On average 41,400 people die of influenza-related illnesses each year in the United States, based on data collected between 1979 and 2001.[181] In industrialised countries, severe illness and deaths occur mainly in the high-risk populations of infants, the elderly and chronically ill patients,[180] although the H1N1 flu outbreak (like the 1918 Spanish flu) differs in its tendency to affect younger, healthier people.[182]
In addition to these annual epidemics, Influenza A virus strains caused three global pandemics during the 20th century: the Spanish flu in 1918, Asian flu in 1957, and Hong Kong flu in 1968–69. These virus strains had undergone major genetic changes for which the population did not possess significant immunity.[183] Recent genetic analysis has revealed that three-quarters, or six out of the eight genetic segments, of the 2009 flu pandemic strain arose from the North American swine flu strains circulating since 1998, when a new strain was first identified on a factory farm in North Carolina, and which was the first-ever reported triple-hybrid flu virus.[184]
The 1918 flu epidemic began with a wave of mild cases in the spring, followed by more deadly waves in the autumn, eventually killing hundreds of thousands in the United States and 50–100 million worldwide.[185] The great majority of deaths in the 1918 flu pandemic were the result of secondary bacterial pneumonia. The influenza virus damaged the lining of the bronchial tubes and lungs of victims, allowing common bacteria from the nose and throat to infect their lungs. Subsequent pandemics have had many fewer fatalities due to the development of antibiotic medicines which can treat pneumonia.[186]
| Pandemic | Year | Influenza virus type | People infected (approximate) | Estimated deaths worldwide | Case fatality rate |
|---|---|---|---|---|---|
| Spanish flu | 1918–1920 | A/H1N1[187] | 33% (500 million)[188] | 50–100 million[189][190][191] | 2–3%[192] |
| Asian flu | 1956–1958 | A/H2N2[187] | ? | 1–4 million[192] | <0.2%[192] |
| Hong Kong flu | 1968–1969 | A/H3N2[187] | ? | 1–4 million[192] | <0.2%[192] |
| Swine flu | 2009–2010 | Pandemic H1N1/09 | 10–200 million[192] | 18,500 (lab-confirmed;[t 1] WHO)[192] – 150,000+ (est. total)[193] | 0.03%[194] |
| Seasonal flu[t 2] | Every year | mainly A/H3N2, A/H1N1, and B | 5–15% (340 million – 1 billion)[195] | 290,000–650,000 per year[180] | <0.1%[196] |
- ^ The ratio of confirmed deaths to total deaths due to pandemic H1N1/09 flu is unknown. For the difficulties in estimating the ratio, see "Data reporting and accuracy"; for some modelling estimates see below.
- ^ Not necessarily pandemic, but included for comparison purposes.
The influenza virus has also caused several pandemic threats over the past century, including the pseudo-pandemic of 1947 (thought of as mild because although globally distributed, it caused relatively few deaths),[183] the 1976 swine flu outbreak and the 1977 Russian flu, all caused by the H1N1 subtype.[183] The world has been at an increased level of alert since the SARS epidemic in Southeast Asia (caused by the SARS coronavirus).[197] The level of preparedness was further increased and sustained with the advent of the H5N1 bird flu outbreaks because of H5N1's high fatality rate, although the strains currently prevalent have limited human-to-human transmission (anthroponotic) capability, or epidemicity.[198]
People who contracted flu before 1957 appeared to have some immunity to H1N1 flu. Daniel Jernigan, head of flu epidemiology for the U.S. CDC, has stated: "Tests on blood serum from older people showed that they had antibodies that attacked the new virus ... That does not mean that everyone over 52 is immune, since Americans and Mexicans older than that have died of the new flu".[199]
In June 2012, a model based study was published finding that the number of deaths related to the H1N1 influenza may have been fifteen times higher than the reported laboratory confirmed deaths. According to their findings, 80% of the respiratory and cardiovascular deaths were in people younger than 65 years and 51% occurred in southeast Asia and Africa. The researchers believe that a disproportionate number of pandemic deaths might have occurred in these regions and that their research suggests that efforts to prevent future influenza pandemics needs to effectively target these regions.[200]
A WHO supported 2013 study estimated that the 2009 global pandemic respiratory mortality was ~10-fold higher than the World Health Organization's laboratory-confirmed mortality count (18.631). Although the pandemic mortality estimate was similar in magnitude to that of seasonal influenza, a marked shift toward mortality among persons <65 y of age occurred, so that many more life-years were lost. Between 123,000 and 203,000 pandemic respiratory deaths were estimated globally for the last 9 mo of 2009. The majority (62%–85%) were attributed to persons under 65 y of age. The burden varied greatly among countries. There was an almost 20-fold higher mortality in some countries in the Americas than in Europe. The model attributed 148,000–249,000 respiratory deaths to influenza in an average pre-pandemic season, with only 19% in persons <65 y.[201]
See also
[edit]- 2009 flu deaths by region
- 2015–16 Zika virus epidemic
- Health crisis
- Public health emergency (United States)
- West African Ebola virus epidemic
References
[edit]- ^ "The Universal Virus Database, version 4: Influenza A". International Committee on Taxonomy of Viruses. Archived from the original on 19 May 2011. Retrieved 14 April 2011.
- ^ Trifonov, Vladimir; Khiabanian, Hossein; Rabadan, Raul (9 July 2009). "Geographic Dependence, Surveillance, and Origins of the 2009 Influenza A (H1N1) Virus". New England Journal of Medicine. 361 (2): 115–19. doi:10.1056/NEJMp0904572. PMID 19474418. S2CID 205105276.
- ^ Hellerman, Caleb (11 June 2009). "Swine flu 'not stoppable,' World Health Organization says". CNN. Archived from the original on 7 March 2010. Retrieved 3 April 2010.
- ^ http://www.cidrap.umn.edu/news-perspective/2011/08/study-puts-global-2009-h1n1-infection-rate-11-21
- ^ "Clinical Aspects of Pandemic 2009 Influenza A (H1N1) Virus Infection". The New England Journal of Medicine. 362 (18): 1708–19. 2010. doi:10.1056/NEJMra1000449. hdl:2381/15212. PMID 20445182.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ a b "Clinical features of severe cases of pandemic influenza". Geneva, CH: World Health Organization (WHO). 16 October 2009. Archived from the original on 25 October 2009. Retrieved 25 October 2009.
- ^ Lin, Rong-Gong II (21 November 2009). "When to take a sick child to the ER". Los Angeles Times. Archived from the original on 25 November 2009. Retrieved 4 January 2010.
- ^ Jain, S & Kamimoto, L (November 2009). "Hospitalized Patients with 2009 H1N1 Influenza in the United States, April–June 2009". N. Engl. J. Med. 361 (20): 1935–44. CiteSeerX 10.1.1.183.7888. doi:10.1056/NEJMoa0906695. PMID 19815859. This study involved a total of 272 patients, which represents approximately 25% of U.S. hospitalized patients with lab-confirmed H1N1 whose cases were reported to the U.S. Centers for Disease Control and Prevention (CDC) from 1 May 2009, to 9 June 2009. The study found that "the only variable that was significantly associated with a positive outcome was the receipt of antiviral drugs within two days after the onset of illness" [Outcomes section, 2nd paragraph] and also that "only 73% of patients with radiographic evidence of pneumonia received antiviral drugs, whereas 97% received antibiotics." [Discussion section, 8th paragraph]. It is recommended that such patients receive both.
- ^ a b c Grady, Denise (3 September 2009). "Report Finds Swine Flu Has Killed 36 Children". The New York Times. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ McNeil, Jr., Donald G. (23 June 2009). "In New Theory, Swine Flu Started in Asia, Not Mexico". The New York Times. Archived from the original on 7 August 2009. Retrieved 1 September 2009.
- ^ "WHO - Swine influenza". Archived from the original on 6 May 2014.
- ^ Chan, Margaret (11 June 2009). "World now at the start of 2009 influenza pandemic". World Health Organization (WHO). Archived from the original on 22 October 2009. Retrieved 25 October 2009.
- ^ a b "2009 H1N1 Flu ("Swine Flu") and You". Centers for Disease Control and Prevention (CDC). 10 February 2010. Archived from the original on 4 March 2010. Retrieved 26 February 2010.
- ^ Huffstutter, P.J. (5 December 2009). "Don't call it 'swine flu,' farmers implore". Los Angeles Times. Archived from the original on 7 December 2009. Retrieved 5 December 2009.
- ^ a b "Updated Interim Recommendations for the Use of Antiviral Medications in the Treatment and Prevention of Influenza for the 2009–2010 Season". H1N1 Flu. Centers for Disease Control and Prevention (CDC). 7 December 2009. Archived from the original on 10 December 2009. Retrieved 10 December 2009.
- ^ Bronze, Michael Stuart (13 November 2009). "H1N1 Influenza (Swine Flu)". eMedicine. Medscape. Archived from the original on 27 December 2009. Retrieved 10 December 2009.
- ^ Mckay, Betsy (2 March 2010). "The Flu Season That Fizzled". The Wall Street Journal. Archived from the original on 17 January 2015. Retrieved 14 April 2011.
- ^ a b "Pandemic (H1N1) 2009 – update 100". Disease Outbreak News. World Health Organization (WHO). 14 May 2010. Archived from the original on 18 May 2010. Retrieved 14 May 2010.
- ^ "Global Intensity Map, Week 17 (April 26, 2010 – 2 May 2010)". Global Update on 2009 H1N1. World Health Organization (WHO). Archived from the original on 19 May 2010. Retrieved 14 May 2010.
- ^ "Percentage of respiratory specimens that tested positive for influenza: Status as of week 17 (25 April 25 – 1 May 2010)". World Health Organization (WHO). Archived from the original on 19 May 2010. Retrieved 14 May 2010.
- ^ "2009 H1N1 Flu: International Situation Update". H1N1 Flu. Centers for Disease Control and Prevention (CDC). 7 May 2010. Archived from the original on 5 May 2010. Retrieved 14 May 2010.
- ^ "WHO/Europe | WHO Director-General declares H1N1 pandemic over". World Health Organization (WHO). 10 August 2010. Archived from the original on 25 May 2011. Retrieved 24 May 2011.
- ^ "WHO | Influenza updates". World Health Organization (WHO). 10 September 2010. Archived from the original on 23 May 2011. Retrieved 24 May 2011.
- ^ "H1N1 Still A Pandemic, Says WHO". redOrbit. Archived from the original on 29 September 2012. Retrieved 10 August 2010.
- ^ "WHO admits errors in handling flu pandemic: Agency accused of overplaying danger of the virus as it swept the globe". MSNBC.com. 12 April 2010. Archived from the original on 12 December 2011. Retrieved 14 April 2011.
- ^ Lynn, Johnathan (12 January 2010). "WHO to review its handling of H1N1 flu pandemic". Reuters. Archived from the original on 24 November 2010. Retrieved 14 April 2011.
- ^ "Swine flu pandemic declared by WHO was 'a waste of money'". London: The Times (UK). 22 April 2010. Archived from the original on 31 May 2010. Retrieved 14 April 2011.
- ^ a b Randall, Tom (7 September 2010). "Swine Flu In Children Found No More Severe Than Seasonal Virus". Bloomberg. Archived from the original on 10 September 2010. Retrieved 30 January 2011.
- ^ Roos, Robert (8 August 2011). "Study puts global 2009 H1N1 infection rate at 11% to 21%". CIDRAP. Archived from the original on 19 August 2012. Retrieved 10 August 2011.
- ^ Dawood FS, Iuliano AD, Reed C, et al. (September 2012). "Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study". Lancet Infect Dis. 12 (9): 687–95. doi:10.1016/S1473-3099(12)70121-4. PMID 22738893.
- ^ "First Global Estimates of 2009 H1N1 Pandemic Mortality Released by CDC-Led Collaboration". Centers for Disease Control and Prevention (CDC). 25 June 2012. Archived from the original on 1 July 2012. Retrieved 3 July 2012.
- ^ "Transcript of virtual press conference with Dr Keiji Fukuda, Assistant Director-General ad Interim for Health Security and Environment, World Health Organization" (PDF). World Health Organization (WHO). 7 July 2009. Archived (PDF) from the original on 6 November 2009. Retrieved 26 October 2009.
- ^ "Interim Novel Influenza A (H1N1) Guidance for Cruise Ships". Centers for Disease Control and Prevention (CDC). 5 August 2009. Archived from the original on 1 October 2009. Retrieved 30 September 2009.
- ^ Kikon, Chonbenthung S. "SWINE FLU: A pandemic". The Morung Express. Archived from the original on 14 July 2011. Retrieved 28 September 2009.
- ^ "Renamed swine flu certain to hit Taiwan". The China Post. Taiwan (ROC). 28 April 2009. Archived from the original on 7 October 2009. Retrieved 26 September 2009.
- ^ Bradsher, Keith (28 April 2009). "The naming of swine flu, a curious matter". The New York Times. Archived from the original on 4 February 2011. Retrieved 29 April 2009.
- ^ Pilkington, Ed (28 April 2009). "What's in a name? Governments debate 'swine flu' versus 'Mexican' flu". The Guardian. London. Archived from the original on 1 May 2009. Retrieved 29 April 2009.
- ^ "CDC Briefing on Investigation of Human Cases of H1N1 Flu". Centers for Disease Control and Prevention (CDC). 24 July 2009. Archived from the original on 29 August 2009. Retrieved 28 July 2009.
- ^ "Interim Guidance for 2009 H1N1 Flu (Swine Flu): Taking Care of a Sick Person in Your Home". Centers for Disease Control and Prevention (CDC). 5 August 2009. Archived from the original on 3 November 2009. Retrieved 1 November 2009.
- ^ Picard, Andre (1 November 2009). "Reader questions on H1N1 answered". The Globe and Mail. Toronto, Canada. Archived from the original on 4 November 2009. Retrieved 2 November 2009.
- ^ Hartocollis, Anemona (27 May 2009). "'Underlying conditions' may add to flu worries". The New York Times. Archived from the original on 25 April 2013. Retrieved 26 September 2009.
- ^ Whalen, Jeanne (15 June 2009). "Flu Pandemic Spurs Queries About Vaccine". The Wall Street Journal. Archived from the original on 7 October 2009. Retrieved 31 August 2009.
- ^ "Surveillance for Pediatric Deaths Associated with 2009 Pandemic Influenza A (H1N1) Virus Infection – United States, April–August 2009". Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention (CDC). 4 September 2009. Archived from the original on 26 November 2009. Retrieved 2 December 2009.
- ^ "2009–2010 Influenza Season Week 6 ending 13 February 2010". Fluview: A Weekly Influenza Surveillance Report Prepared by the Influenza Division. CDC. 15 February 2019. Archived from the original on 19 February 2011.
- ^ "Clinical features of severe cases of pandemic influenza". Pandemic (H1N1) 2009 briefing note 13. Geneva, Switzerland: World Health Organization (WHO). 16 October 2009. Archived from the original on 19 January 2010. Retrieved 17 January 2010.
- ^ Rothberg, MB; Haessler, SD (2010). "Complications of seasonal and pandemic influenza". Critical Care Medicine. 38 (4 Suppl): e91–7. doi:10.1097/CCM.0b013e3181c92eeb. PMID 19935413. S2CID 43882788.
- ^ J.S. Nguyen-Van-Tam, P.J.M. Openshaw, A. Hashim, et al. (2010). "Risk factors for hospitalisation and poor outcome with pandemic A/H1N1 influenza: United Kingdom first wave (May–September 2009)". Thorax. 65 (7): 645–651. doi:10.1136/thx.2010.135210. PMC 2921287. PMID 20627925. Archived from the original on 7 August 2010. Retrieved 21 December 2010.
- ^ Bratincsák, A; El-Said, HG; Bradley, JS; Shayan, K; Grossfeld, PD; Cannavino, CR (10 February 2010). "Fulminant Myocarditis Associated With Pandemic H1N1 Influenza A Virus in Children". Journal of the American College of Cardiology. 55 (9): 928–9. doi:10.1016/j.jacc.2010.01.004. PMID 20153131.
{{cite journal}}: Unknown parameter|lay-url=ignored (help) (primary source) - ^ "Those With Severe H1N1 At Risk For Pulmonary Emboli, Researchers Find". ScienceDaily. 18 October 2009. Archived from the original on 7 March 2010. Retrieved 3 April 2010.
- ^ Belongia, E. A.; Irving, S. A.; Waring, S. C.; Coleman, L. A.; Meece, J. K.; Vandermause, M.; Lindstrom, S.; Kempf, D.; Shay, D. K. (2010). "Clinical Characteristics and 30-Day Outcomes for Influenza A 2009 (H1N1), 2008-2009 (H1N1), and 2007-2008 (H3N2) Infections". Journal of the American Medical Association. 304 (10): 1091–1098. doi:10.1001/jama.2010.1277. PMID 20823435. S2CID 12437691.
- ^ a b "Interim Guidance on Specimen Collection, Processing, and Testing for Patients with Suspected Novel Influenza A (H1N1) Virus Infection". Centers for Disease Control and Prevention (CDC). 13 May 2009. Archived from the original on 26 November 2009. Retrieved 23 November 2009.
- ^ a b "Influenza Diagnostic Testing During the 2009–2010 Flu Season". H1N1 Flu. Centers for Disease Control and Prevention (CDC). 29 September 2009. Archived from the original on 26 November 2009. Retrieved 23 November 2009.
- ^ "Interim Recommendations for Clinical Use of Influenza Diagnostic Tests During the 2009–10 Influenza Season". H1N1 Flu. Centers for Disease Control and Prevention (CDC). 29 September 2009. Archived from the original on 26 November 2009. Retrieved 23 November 2009.
- ^ "Evaluation of Rapid Influenza Diagnostic Tests for Detection of Novel Influenza A (H1N1) Virus --- United States, 2009". Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention (CDC). 7 August 2009. Archived from the original on 17 December 2009. Retrieved 5 December 2009.
- ^ "Accuracy of rapid flu tests questioned". HealthFirst. Mid-Michigan, USA: WJRT-TV/DT. AP. 1 December 2009. Archived from the original on 29 June 2011. Retrieved 5 December 2009.
- ^ "Could Widely Used Rapid Influenza Tests Pose A Dangerous Public Health Risk?". Maywood, Illinois, U.S.: Loyola Medicine. 17 November 2009. Archived from the original on 7 December 2009. Retrieved 4 December 2009.
- ^ a b "Transcript of virtual press conference with Gregory Hartl, Spokesperson for H1N1, and Dr Nikki Shindo, Medical Officer, Global Influenza Programme, World Health Organization" (PDF). World Health Organization (WHO). 12 November 2009. Archived (PDF) from the original on 29 November 2009. Retrieved 18 November 2009.
- ^ "New CDC Test to Detect Human Infections with the 2009 H1N1 Influenza Virus Authorized for Use by FDA" (Press release). Atlanta: Centers for Disease Control and Prevention (CDC). 22 June 2010. Archived from the original on 26 August 2010. Retrieved 25 August 2010.
- ^ Schnirring, Lisa (21 May 2009). "Some immunity to novel H1N1 flu found in seniors". Center for Infectious Disease Research & Policy. Archived from the original on 23 September 2009. Retrieved 26 September 2009.
- ^ "Swine Influenza A (H1N1) Infection in Two Children – Southern California, March–April 2009". Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention (CDC). 21 April 2009. Archived from the original on 25 September 2009. Retrieved 26 September 2009.
- ^ Chen, H; Wang, Y; Liu, W; Zhang, J; Dong, B; Fan, X; De Jong, MD; Farrar, J; Riley, S; Smith, GJD; Guan, Y (2009). "Serologic survey of pandemic (H1N1) 2009 virus, Guangxi Province, China". Emerging Infectious Diseases. 15 (11): 1849–50. doi:10.3201/eid1511.090868. PMC 2857250. PMID 19891883.
- ^ Butler, Declan (29 April 2009). "Swine flu goes global". Nature News. 458 (7242): 1082–1083. doi:10.1038/4581082a. PMID 19407756. S2CID 205044666.
- ^ "Viral gene sequences to assist update diagnostics for swine influenza A(H1N1)" (PDF). World Health Organization. 15 April 2009. Archived (PDF) from the original on 7 August 2017. Retrieved 6 September 2017.
- ^ Emma Wilkinson (1 May 2009). "What scientists know about swine flu". BBC News. Archived from the original on 29 September 2009. Retrieved 26 September 2009.
- ^ Donaldson LJ, Rutter PD, Ellis BM, et al. (2009). "Mortality from pandemic A/H1N1 2009 influenza in England: public health surveillance study". BMJ. 339: b5213. doi:10.1136/bmj.b5213. PMC 2791802. PMID 20007665.
- ^ Maugh, Thomas H. II (11 December 2009). "Swine flu has hit about one in six Americans, CDC says". Los Angeles Times. Archived from the original on 13 December 2009. Retrieved 13 December 2009.
- ^ Vijaykrishna D, Poon LL, Zhu HC, Ma SK, Li OT, Cheung CL, Smith GJ, Peiris JS, Guan Y (18 June 2010). "Reassortment of pandemic H1N1/2009 influenza A virus in swine". Science. 328 (5985): 1529. Bibcode:2010Sci...328.1529V. doi:10.1126/science.1189132. PMC 3569847. PMID 20558710.
- ^ "H1N1 swaps genes with other pig viruses: scientists". CTV News. The Canadian Press. 18 June 2010. Archived from the original on 27 July 2011. Retrieved 14 April 2011.
- ^ Balcan, Duygu; Hu, Hao; Goncalves, Bruno; Bajardi, Paolo; Poletto, Chiara; Ramasco, Jose J.; Paolotti, Daniela; Perra, Nicola; Tizzoni, Michele; Van den Broeck, Wouter; Colizza, Vittoria; Vespignani, Alessandro (14 September 2009). "Seasonal transmission potential and activity peaks of the new influenza A(H1N1): a Monte Carlo likelihood analysis based on human mobility". BMC Medicine. 7 (45): 29. arXiv:0909.2417v1. Bibcode:2009arXiv0909.2417B. doi:10.1186/1741-7015-7-45. PMC 2755471. PMID 19744314.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
- ^ Cauchemez, Simon; Donnelly, Christl A.; Reed, Carrie; Ghani, Azra C.; Fraser, Christophe; Kent, Charlotte K.; Finelli, Lyn; Ferguson, Neil M. (31 December 2009). "Household Transmission of 2009 Pandemic Influenza A (H1N1) Virus in the United States". New England Journal of Medicine. 361 (27): 2619–2627. doi:10.1056/NEJMoa0905498. PMC 3840270. PMID 20042753.
- ^ Murray, Louise (5 November 2009). "Can Pets Get Swine Flu?". The New York Times. Archived from the original on 8 November 2009. Retrieved 6 November 2009.
- ^ Parker-Pope, Tara (5 November 2009). "The Cat Who Got Swine Flu". The New York Times. Archived from the original on 8 November 2009. Retrieved 6 November 2009.
- ^ "Pet dog recovers from H1N1". CBC News. 22 December 2009. Archived from the original on 24 December 2009. Retrieved 14 April 2011.
- ^ "2009 Pandemic H1N1 Influenza Presumptive and Confirmed Results" (PDF). US Department of Agriculture. 4 December 2009. Archived from the original (PDF) on 3 December 2009. Retrieved 4 December 2009.
- ^ "Use of Influenza A (H1N1) 2009 Monovalent Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009" (PDF). Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention (CDC). 28 November 2009. Archived (PDF) from the original on 3 November 2009. Retrieved 2 November 2009.
- ^ a b "Swine flu latest from the NHS". NHS Choices. NHS. NHS Knowledge Service. 25 September 2009. Archived from the original on 8 October 2009. Retrieved 28 September 2009.
- ^ McNeil, Jr., Donald G. (10 September 2009). "One Vaccine Shot Seen as Protective for Swine Flu". The New York Times. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ "Experts advise WHO on pandemic vaccine policies and strategies". World Health Organization (WHO). 30 October 2009. Archived from the original on 2 November 2009. Retrieved 2 November 2009.
- ^ McKay, Betsy (18 July 2009). "New Push in H1N1 Flu Fight Set for Start of School". The Wall Street Journal. Archived from the original on 22 September 2009. Retrieved 31 August 2009.
- ^ Hutain, Jenny (21 November 2009). "478 Community Clinics in 49 States Receiving Needed H1N1 Protective Supplies". Direct Relief. Retrieved 25 April 2019.
- ^ Stickney, R. "Clinics Swamped with Flu Patients". NBC 7 San Diego. Retrieved 25 April 2019.
- ^ "Vaccine Selection for the 2010–2011 Influenza Season". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 6 October 2010. Retrieved 25 August 2010.
- ^ Nasaw, Daniel (27 April 2009). "Europeans urged to avoid Mexico and US as swine flu death toll exceeds 100". Guardian. London. Archived from the original on 30 April 2009. Retrieved 27 April 2009.
- ^ AFP (6 May 2009). "H1N1 virus genome: 'This is a world first'". Independent. Archived from the original on 7 October 2009. Retrieved 31 August 2009.
- ^ "National Pandemic Flu Service". NHS, NHS Scotland, NHS Wales, DHSSPS. Archived from the original on 7 October 2009. Retrieved 4 October 2009.
- ^ Hines, Lora (7 June 2009). "Health officials evaluate response to swine flu". Riverside Press-Enterprise. Archived from the original on 7 January 2010. Retrieved 17 September 2009.
- ^ Stein, Rob (10 August 2009). "Preparing for Swine Flu's Return". The Washington Post. Archived from the original on 7 October 2009. Retrieved 4 October 2009.
- ^ a b Steenhuysen, Julie (4 June 2009). "As swine flu wanes, U.S. preparing for second wave". Reuters. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ Shear, Michael D.; Stein, Rob (24 October 2009). "President Obama declares H1N1 flu a national emergency". The Washington Post. Archived from the original on 7 November 2009. Retrieved 25 October 2009.
- ^ Fineberg, Harvey V. (3 April 2014). "Pandemic Preparedness and Response — Lessons from the H1N1 Influenza of 2009". NEJM. 370 (14): 1335–1342. doi:10.1056/NEJMra1208802. PMID 24693893.
- ^ Pollard, Chris (13 January 2010). "Swine flu 'a false pandemic' to sell vaccines, expert says". News.com. Archived from the original on 14 January 2010. Retrieved 13 January 2010.
- ^ "WHO to review its handling of H1N1 flu pandemic". Reuters. 12 January 2010. Archived from the original on 24 November 2010. Retrieved 14 April 2011.
- ^ Bloomberg Bloomberg News https://www.bloomberg.com/apps/news?pid=20601091&sid=ahj0H_RH8U68. Archived from the original on 7 March 2010. Retrieved 21 August 2017.
{{cite web}}: Missing or empty|title=(help) - ^ Flynn, Paul (23 March 2010). "The handling of the H1N1 pandemic: more transparency needed" (PDF). memorandum, Social, Health and Family Affairs Committee, The Council of Europe. Archived (PDF) from the original on 23 February 2011.
- ^ a b Chan M (8 June 2010). "WHO Director-General's letter to BMJ editors". World Health Organization (WHO). Archived from the original on 30 January 2011. Retrieved 30 January 2011.
- ^ Fiona Godlee (2010). "Conflicts of interest and pandemic flu". BMJ. 340: c2947. doi:10.1136/bmj.c2947. PMID 20525680. S2CID 323055. Archived from the original on 21 December 2010. Retrieved 21 December 2010.
- ^ "WHO – Influenza A(H1N1) – Travel". World Health Organization (WHO). 7 May 2009. Archived from the original on 18 June 2009. Retrieved 17 June 2009.
- ^ "FACTBOX-Asia moves to ward off new flu virus". Reuters. 9 February 2009. Archived from the original on 30 April 2009. Retrieved 26 April 2009.
- ^ a b c Jacobs, Karen (3 June 2009). "Global airlines move to reduce infection risks". Reuters. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ Gunaratnam, P.J.; Tobin, S.; Seale, H.; Marich, A.; McAnulty, J. (17 March 2014). "Airport arrivals screening during pandemic (H1N1) 2009 influenza in New South Wales, Australia". Medical Journal of Australia. 200 (5): 290–292. doi:10.5694/mja13.10832. PMID 24641156. S2CID 43883770.
- ^ Nishiura, H.; Kamiya, K. (3 May 2011). "Fever screening during the influenza (H1N1-2009) pandemic at Narita International Airport, Japan". BMC Infectious Diseases. 11: 111. doi:10.1186/1471-2334-11-111. PMC 3096599. PMID 21539735.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "New CDC H1N1 Guidance for Colleges, Universities, and Institutions of Higher Education". Business Wire. 20 August 2009. Retrieved 17 September 2009.
- ^ a b George, Cindy (1 August 2009). "Schools revamp swine flu plans for fall". Houston Chronicle. Archived from the original on 7 October 2009. Retrieved 31 August 2009.
- ^ de Vise, Daniel (20 August 2009). "Colleges Warned About Fall Flu Outbreaks on Campus". The Washington Post. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ "Get Smart About Swine Flu for Back-to-School". Atlanta Journal-Constitution. 14 August 2009. Archived from the original on 7 October 2009. Retrieved 31 August 2009.
- ^ a b Mehta, Seema; Nicole Santa Cruz (27 July 2009). "Swine flu goes to camp. Will it go to school next?". Los Angeles Times. Archived from the original on 7 August 2009. Retrieved 17 September 2009.
- ^ James C. Jr., King (1 August 2009). "The ABC's of H1N1". The New York Times. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ "H1N1 Closes Hundreds of Schools Across the U.S." Fox News. 28 October 2009. Archived from the original on 1 November 2009. Retrieved 28 October 2009.
- ^ a b "Business Planning". Flu.gov. U.S. Department of Health & Human Services. Archived from the original on 30 August 2009. Retrieved 17 September 2009.
- ^ Maugh II, Thomas H. (25 July 2009). "Swine flu could kill hundreds of thousands in U.S. if vaccine fails, CDC says". Los Angeles Times. Archived from the original on 7 August 2009. Retrieved 17 September 2009.
- ^ Fiore, Marrecca (17 July 2009). "Swine Flu: Why You Should Still Be Worried". Fox News. Archived from the original on 9 September 2009. Retrieved 31 August 2009.
- ^ "Swine flu – HSE News Announcement". Health and Safety Executive. 18 June 2009. Archived from the original on 27 August 2009. Retrieved 31 August 2009.
- ^ Roan, Shari (27 September 2009). "Masks may help prevent flu, but aren't advised". Chicago Tribune. Archived from the original on 1 October 2009. Retrieved 28 September 2009.
- ^ a b c Roan, Shari; Rong-Gong Lin II (30 April 2009). "Face masks aren't a sure bet against swine flu". Los Angeles Times. Archived from the original on 3 May 2009. Retrieved 17 September 2009.
- ^ a b c "Face masks part of Japan fashion chic for decades". Bangkok Post. The Post Publishing. AFP. 5 April 2009. Retrieved 28 October 2009.[dead link]
- ^ Wohl, Jessica (20 October 2009). "Flu-Related Products May Lift U.S. Makers' Profits". ABC News.com. ABC News. Archived from the original on 24 October 2009. Retrieved 28 October 2009.
- ^ "China quarantines U.S. school group over flu concerns". CNN. 28 May 2009. Archived from the original on 7 October 2009. Retrieved 26 September 2009.
- ^ Kralev, Nicholas (29 June 2009). "KRALEV: U.S. warns travelers of China's flu rules". The Washington Times. Archived from the original on 7 October 2009. Retrieved 26 September 2009.
- ^ DPA (3 May 2009). "Tensions escalate in Hong Kong's swine-flu hotel". Taipei Times. Archived from the original on 7 November 2009. Retrieved 26 September 2009.
- ^ "Ship passengers cruisy in swine flu quarantine". ABC News. Australian Broadcasting Corporation. 28 May 2009. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ Anonymous (21 May 2009). "Egypt warns of post-hajj swine flu quarantine". Philippine Star. Archived from the original on 29 August 2014. Retrieved 16 October 2013.
- ^ Woolls, Daniel (27 April 2009). "Swine flu cases in Europe; worldwide travel shaken". The America's Intelligence Wire. AP. Retrieved 30 January 2011.
- ^ "Japan Swine Flu Quarantine Ends for Air Passengers". New Tang Dynasty Television. 17 May 2009. Archived from the original on 7 December 2009. Retrieved 26 September 2009.
- ^ MIL/Sify.com (16 June 2009). "India wants US to screen passengers for swine flu". International Reporter. Archived from the original on 23 September 2010. Retrieved 28 September 2009.
- ^ Jordan, Dave (20 October 2009). "Minnesota Pig Tests Positive for H1N1". KOTV. Archived from the original on 7 December 2009. Retrieved 10 December 2009.
- ^ Evans, Brian (5 May 2009). "News Conference with Minister of Health and Chief Public Health Officer". Public Health Agency of Canada. Archived from the original on 14 December 2009. Retrieved 10 December 2009.
- ^ "Human swine flu in pigs". Effect Measure. 20 October 2009. Archived from the original on 8 November 2009. Retrieved 10 December 2009.
- ^ "Joint FAO/WHO/OIE Statement on influenza A(H1N1) and the safety of pork" (Press release). World Health Organization (WHO). 7 May 2009. Archived from the original on 23 September 2009. Retrieved 26 September 2009.
- ^ Desmon, Stephanie (21 August 2009). "Pork industry rues swine flu". The Baltimore Sun. Vol. 172, no. 233. pp. 1, 16. Archived from the original on 7 October 2009. Retrieved 1 September 2009.
- ^ "Prevention against "swine flu" stabile in Azerbaijan: minister". Trend News Agency. 28 April 2009. Archived from the original on 16 July 2009. Retrieved 28 April 2009.
- ^ "Cegah flu babi, pemerintah gelar rapat koordinasi". Kompas newspaper. 27 April 2009. Archived from the original on 1 May 2009. Retrieved 14 April 2011.
- ^ "Egypt orders pig cull". ABC News. Australian Broadcasting Corporation. AFP. 30 April 2009. Archived from the original on 7 October 2009. Retrieved 27 September 2009.
- ^ a b Mayo Clinic Staff. "Influenza (flu) treatments and drugs". Diseases and Conditions. Mayo Clinic. Archived from the original on 7 October 2009. Retrieved 20 May 2009.
- ^ a b "Fever". Medline Plus Medical Encyclopedia. U.S. National Library of Medicine. Archived from the original on 15 May 2009. Retrieved 20 May 2009.
- ^ "Aspirin / Salicylates and Reyes Syndrome". National Reye's Syndrome Foundation. 1974. Archived from the original on 19 July 2011. Retrieved 14 April 2011.
- ^ "What To Do If You Get Sick: 2009 H1N1 and Seasonal Flu". Centers for Disease Control and Prevention (CDC). 7 May 2009. Archived from the original on 3 November 2009. Retrieved 1 November 2009.
- ^ Jain S, Kamimoto L, Bramley AM, et al. (November 2009). "Hospitalized patients with 2009 H1N1 influenza in the United States, April–June 2009". New England Journal of Medicine. 361 (20): 1935–44. CiteSeerX 10.1.1.183.7888. doi:10.1056/NEJMoa0906695. PMID 19815859.
- ^ "Emergency Use Authorization Granted For BioCryst's Peramivir". PRNewswire. PRNewswire-FirstCall. 23 October 2009. Archived from the original on 6 June 2011. Retrieved 30 January 2011.
- ^ Cheng, Maria (21 August 2009). "WHO: Healthy people who get swine flu don't need Tamiflu; drug for young, old, pregnant". Washington Examiner. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ BMJ Group (8 May 2009). "Warning against buying flu drugs online". Boots. Archived from the original on 17 October 2013. Retrieved 16 October 2013.
- ^ "Update on oseltamivir resistance to influenza H1N1 (2009) viruses" (PDF). World Health Organization (WHO). 15 December 2010. Archived (PDF) from the original on 27 January 2011. Retrieved 30 December 2010.
- ^ "2008–2009 Influenza Season Week 39 ending October 3, 2009". Centers for Disease Control and Prevention (CDC). 9 October 2009. Archived from the original on 6 March 2010. Retrieved 20 November 2009.
- ^ "2008–2009 Influenza Season Week 32 ending August 15, 2009". Flu Activity & Surveillance. Centers for Disease Control and Prevention (CDC). 21 August 2009. Archived from the original on 3 November 2009. Retrieved 4 December 2009.
- ^ Cortez, Michelle Fay (9 December 2009). "Roche's Tamiflu Not Proven to Cut Flu Complications, Study Says". Bloomberg L.P. Archived from the original on 7 January 2010. Retrieved 11 December 2009.
- ^ a b c Jefferson, Tom; Jones, Mark; Doshi, Peter; Del Mar, Chris (8 December 2009). "Neuraminidase inhibitors for preventing and treating influenza in healthy adults: systematic review and meta-analysis". BMJ. 339: b5106. doi:10.1136/bmj.b5106. PMC 2790574. PMID 19995812. Retrieved 11 December 2009.
- ^ Godlee, Fiona (10 December 2009). "We want raw data, now". BMJ. 339: b5405. doi:10.1136/bmj.b5405. S2CID 72788639. Archived from the original on 7 March 2010. Retrieved 14 April 2011.
- ^ a b Check, Hayden Erica (5 May 2009). "The turbulent history of the A(H1N1) virus". Nature. 459 (7243): 14–5. doi:10.1038/459014a. ISSN 1744-7933. PMC 7095218. PMID 19424121.
- ^ Larry Pope. Smithfield Foods CEO on flu virus (flv) (Television production). NBC News. Retrieved 16 September 2009.
- ^ Cohen Jon; Enserink Martin (1 May 2009). "As Swine Flu Circles Globe, Scientists Grapple With Basic Questions". Science. 324 (5927): 572–3. doi:10.1126/science.324_572. PMID 19407164.
- ^ Fox, Maggie (11 June 2009). "New flu has been around for years in pigs – study". Reuters. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ a b McNeil Jr., Donald G. (26 April 2009). "Flu Outbreak Raises a Set of Questions". The New York Times. Archived from the original on 15 February 2011. Retrieved 17 September 2009.
- ^ a b "Study: Mexico Has Thousands More Swine Flu Cases". Fox News Network. Associated Press. 12 May 2009. Archived from the original on 24 September 2009. Retrieved 17 September 2009.
- ^ "Swine Influenza A (H1N1) Infection in Two Children --- Southern California, March–April 2009". Morbidity and Mortality Weekly Report. 58 (Dispatch) (15). Centers for Disease Control and Prevention (CDC): 400–402. 24 April 2009. Archived from the original on 1 October 2009. Retrieved 4 October 2009.
- ^ "Swine flu victim dies in Houston". Houston, Texas: KTRK-TV/DT. AP. 29 April 2009. Archived from the original on 7 November 2009. Retrieved 18 November 2009.
- ^ "Pandemic reveals strengths of new flu database". CIDRAP. Retrieved 6 September 2017.
- ^ Elbe, Stefan; Buckland-Merrett, Gemma (1 January 2017). "Data, disease and diplomacy: GISAID's innovative contribution to global health". Global Challenges. 1 (1): 33–46. doi:10.1002/gch2.1018. ISSN 2056-6646. PMC 6607375. PMID 31565258.
- ^ Greenemeier, Larry. "Building a Better Flu Vaccine--and Giving Chickens a Rest". Scientific American. Archived from the original on 6 September 2017. Retrieved 6 September 2017.
- ^ McCauley, John W. (23 February 2017). "Viruses: Model to accelerate epidemic responses". Nature. 542 (7642): 414. Bibcode:2017Natur.542..414M. doi:10.1038/542414b. PMID 28230113. S2CID 52869054.
- ^ "Flu Activity & Surveillance". Centers for Disease Control and Prevention (CDC). 30 November 2009. Archived from the original on 26 November 2009. Retrieved 2 December 2009.
- ^ Stobbe, Mike (25 June 2009). "US Swine Flu Cases May Have Hit 1 Million". The Huffington Post. AP. Archived from the original on 7 December 2009. Retrieved 2 December 2009.
- ^ Ellenberg, Jordan (4 July 2009). "Influenza Body Count". Slate. Archived from the original on 15 January 2010. Retrieved 2 December 2009.
- ^ "Questions and Answers Regarding Estimating Deaths from Influenza in the United States". Seasonal Influenza (Flu). Centers for Disease Control and Prevention (CDC). 4 September 2009. Archived from the original on 1 December 2009. Retrieved 2 December 2009.
- ^ "CDC Estimates of 2009 H1N1 Influenza Cases, Hospitalizations and Deaths in the United States, April – December 12, 2009". H1N1 Flu. CDC. 15 January 2010. Archived from the original on 19 January 2010. Retrieved 17 January 2010.
- ^ "CDC week 45". Centers for Disease Control and Prevention (CDC). 14 November 2009. Archived from the original on 7 January 2010. Retrieved 14 December 2009.
- ^ "CDC week 34". Centers for Disease Control and Prevention (CDC). 30 August 2009. Archived from the original on 7 January 2010. Retrieved 14 December 2009.
- ^ Gale, Jason (4 December 2009). "Clinical features of severe cases of pandemic influenza". Bloomberg. Archived from the original on 7 January 2010. Retrieved 4 December 2009.
- ^ "GLOBAL: No A (H1N1) cases – reality or poor lab facilities?". Reuters. 8 May 2009. Archived from the original on 11 May 2009. Retrieved 9 May 2009.
- ^ Sandman, Peter M.; Lanard, Jody (2005). "Bird Flu: Communicating the Risk". Perspectives in Health Magazine. 10 (2). Archived from the original on 23 April 2011. Retrieved 14 April 2011.
- ^ "Pandemic (H1N1) 2009 briefing note 3". World Health Organization (WHO). Archived from the original on 22 July 2009. Retrieved 17 July 2009.
- ^ Randall, Tom (7 September 2010). "Swine Flu Found No More Severe Than Seasonal Virus". Bloomberg. Archived from the original on 10 September 2010. Retrieved 24 May 2011.
- ^ "Updated CDC Estimates of 2009 H1N1 Influenza Cases, Hospitalizations and Deaths in the United States, April 2009 – April 10, 2010". Cdc.gov. Archived from the original on 9 December 2010. Retrieved 24 May 2011.
- ^ Sundar S. Shrestha; David L. Swerdlow; Rebekah H. Borse; Vimalanand S. Prabhu; Lyn Finelli; Charisma Y. Atkins; Kwame Owus-Edusei; Beth Bell; Paul S. Mead; Matthew Biggerstaff; Lynnette Brammer; Heidi Davidson; Daniel Jernigan; Michael A. Jhung; Laurie A. Kamimoto; Toby L. Merlin; Mackenzie Nowell; Stephen C. Redd; Carrie Reed; Anne Schuchat; Martin I. Meltzer (2011). "Estimating the Burden of 2009 Pandemic Influenza A (H1N1) in the United States (April 2009–April 2010)". Clinical Infectious Diseases. 52 (suppl 1): S75–S82. doi:10.1093/cid/ciq012. PMID 21342903.
- ^ "Flu Season Continues; Severity Indicators Rise". Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases (NCIRD). 17 January 2014. Archived from the original on 21 January 2014. Retrieved 24 January 2014.
- ^ Mason, Michael. "Flu – Symptoms, Diagnosis, Treatment of Flu – NY Times Health Information". The New York Times. Archived from the original on 14 July 2011. Retrieved 24 May 2011.
- ^ "CDC - Seasonal Influenza (Flu) - Questions and Answers Regarding Estimating Deaths from Influenza in the United States". Cdc.gov. Archived from the original on 16 October 2011. Retrieved 23 October 2011.
- ^ "CDC Estimates of 2009 H1N1 Influenza Cases, Hospitalizations and Deaths in the United States, April – November 14, 2009". Flu.gov. Archived from the original on 9 December 2011. Retrieved 23 October 2011.
- ^ Scarfone, Richard J.; Susan Coffin; Evan S. Fieldston; Grace Falkowski; Mary G. Cooney; Stephanie Grenfell (June 2011). "Hospital-Based Pandemic Influenza Preparedness and Response: Strategies to Increase Surge Capacity". Pediatric Emergency Care. 27 (6): 565–572. doi:10.1097/PEC.0b013e31821dc9d1. PMID 21642799. S2CID 11222604.
- ^ a b c "Influenza: Fact sheet". World Health Organization (WHO). 6 November 2018. Archived from the original on 17 December 2019. Retrieved 25 January 2020.
- ^ Dushoff, J.; Plotkin, J. B.; Viboud, C.; Earn, D. J. D.; Simonsen, L. (2006). "Mortality due to Influenza in the United States – An Annualized Regression Approach Using Multiple-Cause Mortality Data". American Journal of Epidemiology. 163 (2): 181–7. doi:10.1093/aje/kwj024. PMID 16319291.
The regression model attributes an annual average of 41,400 (95% confidence interval: 27,100, 55,700) deaths to influenza over the period 1979–2001.
- ^ Kaplan, Karen (18 September 2009). "Swine flu's tendency to strike the young is causing confusion". Los Angeles Times. Archived from the original on 19 September 2009. Retrieved 18 September 2009.
- ^ a b c Kilbourne, ED; Zhang, Yan B.; Lin, Mei-Chen (January 2006). "Influenza pandemics of the 20th century". Emerging Infectious Diseases. 12 (1): 9–14. doi:10.3201/eid1201.051254. PMC 3291411. PMID 16494710.
- ^ Greger, Michael (26 August 2009). "CDC Confirms Ties to Virus First Discovered in U.S. Pig Factories". The Humane Society of the United States. Archived from the original on 3 September 2009. Retrieved 21 September 2009.
- ^ Sternberg, Steve (26 May 2009). "CDC expert says flu outbreak is dying down – for now". USA Today. Archived from the original on 7 October 2009. Retrieved 17 September 2009.
- ^ David M. Morens; Jeffery K. Taubenberger; Anthony S. Fauci (1 October 2008). "Predominant Role of Bacterial Pneumonia as a Cause of Death in Pandemic Influenza: Implications for Pandemic Influenza Preparedness". The Journal of Infectious Diseases. 198 (7): 962–970. doi:10.1086/591708. PMC 2599911. PMID 18710327.
- ^ a b c Hsieh, Yu-Chia; et al. (January 2006). "Influenza pandemics: past present and future" (PDF). Journal of the Formosan Medical Association. 105 (1): 1–6. doi:10.1016/S0929-6646(09)60102-9. PMID 16440064. Archived from the original (PDF) on 7 August 2009. Retrieved 26 September 2009.
- ^ Taubenberger, Jeffery K.; Morens, David M. (January 2006). "1918 Influenza: the Mother of All Pandemics". Emerging Infectious Diseases. 12 (1): 15–22. doi:10.3201/eid1201.050979. PMC 3291398. PMID 16494711.
- ^ Institute of Medicine (US) Forum on Microbial Threats, Knobler SL, Mack A, Mahmoud A, Lemon SM (2005). "1: The Story of Influenza". In Knobler S, Mack A, Mahmoud A, Lemon S (eds.). The Threat of Pandemic Influenza: Are We Ready? Workshop Summary (2005). Washington, D.C.: The National Academies Press. pp. 60–61. doi:10.17226/11150. ISBN 978-0-309-09504-4. PMID 20669448. Retrieved 26 September 2009.
- ^ Patterson, KD; Pyle GF (Spring 1991). "The geography and mortality of the 1918 influenza pandemic". Bull Hist Med. 65 (1): 4–21. PMID 2021692.
- ^ "Ten things you need to know about pandemic influenza". World Health Organization (WHO). 14 October 2005. Archived from the original on 6 August 2010. Retrieved 26 September 2009.
- ^ a b c d e f g "Report of the Review Committee on the Functioning of the International Health Regulations (2005) in relation to Pandemic (H1N1) 2009" (PDF). 5 May 2011. Archived (PDF) from the original on 14 May 2015. Retrieved 1 March 2015.
- ^ "No more flu shot? Search begins for universal influenza vaccine". Fox News. 13 January 2017. Archived from the original on 6 February 2017.
- ^ Triggle, Nick (10 December 2009). "Swine flu less lethal than feared". BBC News. BBC. Archived from the original on 13 December 2009. Retrieved 10 December 2009.
- ^ "WHO Europe – Influenza". World Health Organization (WHO). June 2009. Archived from the original on 17 June 2009. Retrieved 12 June 2009.
- ^ "H1N1 fatality rates comparable to seasonal flu". The Malaysian Insider. Washington, D.C., USA. Reuters. 17 September 2009. Archived from the original on 20 October 2009. Retrieved 26 September 2009.
- ^ Brown, David (29 April 2009). "System set up after SARS epidemic was slow to alert global authorities". The Washington Post. Retrieved 26 September 2009.
- ^ Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, Lochindarat S, Nguyen TK, Nguyen TH, Tran TH, Nicoll A, Touch S, Yuen KY (29 September 2005). "Avian influenza A (H5N1) infection in humans". The New England Journal of Medicine. 353 (13). Writing Committee of the World Health Organization (WHO) Consultation on Human Influenza A/H5: 1374–85. CiteSeerX 10.1.1.730.7890. doi:10.1056/NEJMra052211. PMID 16192482.
- ^ McNeil Jr., Donald G. (20 May 2009). "U.S. Says Older People Appear Safer From New Flu Strain". The New York Times. Archived from the original on 7 October 2009. Retrieved 26 September 2009.
- ^ "H1N1 Swine Flu May Have Killed 15 Times More Than First Said". ABC News Medical Unit. 26 June 2012. Archived from the original on 20 March 2016., citing Dawood FS, Iuliano AD, et al. (26 June 2012). "Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study". The Lancet Infectious Diseases. 12 (9): 687–95. doi:10.1016/S1473-3099(12)70121-4. PMID 22738893.
- ^ Simonsen, Lone; Spreeuwenberg, Peter; Lustig, Roger; Taylor, Robert J.; Fleming, Douglas M.; Kroneman, Madelon; Van Kerkhove, Maria D.; Mounts, Anthony W.; Paget, W. John; Hay, Simon I. (26 November 2013). "Global Mortality Estimates for the 2009 Influenza Pandemic from the GLaMOR Project: A Modeling Study". PLOS Medicine. 10 (11): e1001558. doi:10.1371/journal.pmed.1001558. PMC 3841239. PMID 24302890.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
Further reading
[edit]- Cannell, JJ; Zasloff, M; Garland, CF; Scragg, R; Giovannucci, E (25 February 2008). "On the epidemiology of influenza". Virology Journal. 5 (1): 29. doi:10.1186/1743-422X-5-29. PMC 2279112. PMID 18298852.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - MacPhail, Theresa (2014). The Viral Network. Ithaca, London: Cornell University Press. ISBN 978-0-8014-7983-0.
- Smith, GJ; et al. (25 June 2009). "Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic". Nature. 459 (7250): 1122–1125. Bibcode:2009Natur.459.1122S. doi:10.1038/nature08182. PMID 19516283. S2CID 57894.
- Soundararajan, V; et al. (June 2009). "Extrapolating from sequence—the 2009 H1N1 'swine' influenza virus". Nature Biotechnology. 27 (6): 510–513. doi:10.1038/nbt0609-510. PMID 19513050. S2CID 22710439.
- Centers for Disease Control and Prevention (CDC) (October 2009). "Introduction and transmission of 2009 pandemic influenza A (H1N1) Virus—Kenya, June–July 2009". Morbidity and Mortality Weekly Report. 58 (41): 1143–6. PMID 19847148. Archived from the original on 13 May 2011. Retrieved 14 April 2011.
External links
[edit]- Pandemic (H1N1) 2009 at the World Health Organization (WHO)
- International Society for Infectious Diseases PROMED-mail news updates
- H1N1 Flu Resource Centre of The Lancet
- Novel H1N1 Influenza (Swine Flu) Overview from CIDRAP
- Influenza Research Database – Database of influenza genomic sequences and related information.
- CDC 2009 H1N1 Influenza Vaccine Supply Status
- The H1N1 Pandemic and Global Health Security, Dean Julio Frenk, 2009-09-17
- Health-EU Portal EU response to influenza
- 2009 influenza A (H1N1) pandemic. European Centre for Disease Prevention and Control (ECDC).
- Summaries of the pandemic. European Centre for Disease Prevention and Control (ECDC).
- European Commission – Public Health EU coordination on Pandemic (H1N1) 2009.
- UK National Pandemic Flu Service
- Official UK government information on swine flu from Directgov
- Human/Swine A/H1N1 Influenza Origins and Evolution – Analysis of genetic data for the origin and evolution of swine flu virus.
- Health Canada flu portal
- Pan-American Health Organization (PAHO) Swine Influenza portal
- H1N1 Influenza (Flu) portal at the US Centers for Disease Control (CDC)
- US Government swine, avian and pandemic flu portal
- Medical Encyclopedia Medline Plus: Swine Flu
- Swine Flu Outbreak, Influenza Virus Resource – Sequences and related resources (GenBank, NCBI)
Template:Good article is only for Wikipedia:Good articles.
