User:Mpagan2/Sandbox
From Userpage
[edit]Mechanism of action
[edit]The mechanism of thalidomide's teratogenic action has led to over 2000 research papers and the proposal of 15 or 16 plausible mechanisms.[1] Angiogenesis is critical during limb development of the foetus. In 1998, it was found in vivo that during limb development thalidomide was able to inhibit the stimulatory effects of growth factors FGF-2 and IGF-1 [2] that promote angiogenesis. Surface integrin αVβ3 is notably important in this process. Previous work showed thalidomide's ability to decrease integrin production on the cell surface, decreasing the cell's ability to stimulate new blood vessels, and inhibit angiogenesis stimulated by FGF-2.[3][4] It was soon found that αVβ3 had several GC box sequences in its promoter region and the same was true for FGF-2 and IGF-1 and their receptors on the cell surface.[5][6][7][8][9][10][11] Further investigation into this phenomenon found that at least eight other proteins in the growth-stimulating cascade too had promotors containing this region.[1][12] Thalidomide has a high affinity for guanine, thus it was hypothesized that thalidomide intercalates into these GC boxes and prevents integrins from stimulating new blood vessels that support limb development, thereby exerting the tetratogenic effects seen in thalidomide-induced birth defects.[1][12]
In 2009, research by other groups confirmed "conclusively that loss of newly formed blood vessels is the primary cause of thalidomide teratogenesis, and developing limbs are particularly susceptible because of their relatively immature, highly angiogenic vessel network".[13][14]
TNF-α
[edit]Tumor necrosis factor alpha (TNF-α) is a cytokine that is chiefly involved in regulating white blood cells. Changes in the regulation of this protein has been found to be related to various diseases such as Alzheimer's disease[15] and cancer.[16]
In 1990, a group of researchers in Brazil noted that TNF-α levels went up in leprosy reactional states and observed that TNF levels decreased in some patients on treatment with thalidomide, hence potentially explaining the efficacy of thalidomide in treating ENL.[17]
In light of this, further study of how this drug affected TNF-α were conducted. In 1993, thalidomide was found to selectively degrade TNF-α mRNA[18], however how it does so is unclear. This is compared to other known TFN-α inhibitors, some of which have been found to block transcription of the TNF-α gene[19], TNFA, or block translation of the mRNA.[20] Further, this reduction in TNF-α lead to a decrease in inflammatory cytokine levels, suggesting thalidomide's use in treating other inflammatory infections.
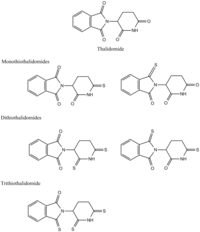
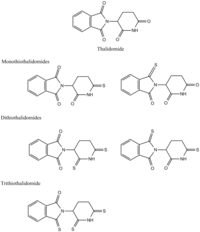
Thalidomide analogs have been found to have even more profound effects on TNF-α inhibition than their parent molecule. Replacing thalidomide's carbonyls with thiones increased its ability to inhibit TNF-α[21] in the following order:
trithiothalidomide > dithiothalidomide > monothiothalidomide > thalidomide
as seen in the structures to the right. It is hypothesized that this these analogs act on the 3'-UTR of TNFA to exert their effects.
Synthesis
[edit]Thalidomide is synthesized into a racemic mixture, however separating the mixture into a enatiomerically pure solution would prove fruitless[22][23][24] as the racemization can occur in vivo.[25][26][22][27] Celgene Corporation originally synthesized thalidomide using a three-step sequence starting with L-glutamic acid treatment, but this has since been reformed by the use of L-glutamine.[28] As shown in the image below, N-carbethoxyphtalimide (1) can react with L-glutamine to yield N-Phthaloyl-L-glutamine (2). Cyclization of N-Phthaloyl-L-glutamine occurs using carbonyldiimidazole, which then yields thalidomide (3).[28] Celegne Corporation's original method resulted in a 31% yield of S-thalidomide, whereas the two-step synthesis yields 85-93% product that is 99% pure.

From article
[edit]Mechanism of action
[edit]The precise mechanism of action for thalidomide is unknown, but possible mechanisms include anti-angiogenic and oxidative stress-inducing effects.[29] It also inhibits TNF-α, IL-6, IL-10 and IL-12 production,[30] modulates the production of IFN-γ[30] and enhances the production of IL-2, IL-4 and IL-5 by immune cells.[30] It increases lymphocyte count, costimulates T cells and modulates natural killer cell cytotoxicity.[30] It also inhibits NF-κB and COX-2 activity.[29]
The mechanism of thalidomide's teratogenic action has led to over 2000 research papers and the proposal of 15 or 16 plausible mechanisms.[1] Angiogenesis is critical during limb development of the foetus. In 1998, it was found in vivo that during limb development thalidomide was able to inhibit the stimulatory effects of growth factors FGF-2 and IGF-1[2] that promote angiogenesis. Surface integrin αVβ3 is notably important in this process. Previous work showed thalidomide's ability to decrease integrin production on the cell surface, decreasing the cell's ability to stimulate new blood vessels, and inhibit angiogenesis stimulated by FGF-2.[3][4] It was soon found that αVβ3 had several GC box sequences in its promoter region and the same was true for FGF-2 and IGF-1 and their receptors on the cell surface.[5][6][7][8][9][10][11] Further investigation into this phenomenon found that at least eight other proteins in the growth-stimulating cascade too had promotors containing this region.[1][12] Thalidomide has a high affinity for guanine, thus it was hypothesized that thalidomide intercalates into these GC boxes and prevents integrins from stimulating new blood vessels that support limb development, thereby exerting the tetratogenic effects seen in thalidomide-induced birth defects. [1][12]
In 2009, research by other groups confirmed "conclusively that loss of newly formed blood vessels is the primary cause of thalidomide teratogenesis, and developing limbs are particularly susceptible because of their relatively immature, highly angiogenic vessel network".[13][14]

Left: (S)-(−)-thalidomide
Right: (R)-(+)-thalidomide
Thalidomide is racemic; the individual enantiomers can racemize due to the acidic hydrogen at the chiral centre, which is the carbon of the glutarimide ring bonded to the phthalimide substituent. The racemization process can occur in vivo[25][26][22][27] so that any plan to administer a purified single enantiomer to avoid the teratogenic effects will most likely be in vain.[22][23][24]
TNF-α
[edit]Tumor necrosis factor alpha (TNF-α) is a cytokine that is chiefly involved in regulating white blood cells. Changes in the regulation of this protein has been found to be related to various diseases such as Alzheimer's disease[31] and cancer.[32].
In 1990, a group of researchers in Brazil noted that TNF-α levels went up in leprosy reactional states and observed that TNF levels decreased in some patients on treatment with thalidomide, hence potentially explaining the efficacy of thalidomide in treating ENL.[33]
In light of this, further study of how this drug affected TNF-α were conducted. In 1993, thalidomide was found to selectively degrade TNF-α mRNA[34], however how it does so is unclear. This is compared to other known TFN-α inhibitors, some of which have been found to block transcription of the TNF-α gene[35], TNFA, or block translation of the mRNA.[36] Further, this reduction in TNF-α lead to a decrease in inflammatory cytokine levels, suggesting thalidomide's use in treating other inflammatory infections.
Thalidomide analogs have been found to have even more profound effects on TNF-α inhibition than their parent molecule. Replacing thalidomide's carbonyls with thiones increased its ability to inhibit TNF-α[37] in the following order:
trithiothalidomide > dithiothalidomide > monothiothalidomide > thalidomide
as seen in the structures to the right. It is hypothesized that this these analogs act on the 3'-UTR of TNFA to exert their effects.
Cereblon
[edit]Several studies have shown that the mechanism of action for thalidomide involves binding to the protein cereblon, a ubiquitin ligase substrate adapter protein,[38] which is important in limb formation[39] and the proliferative capacity of myeloma cells. Ubiquitin ligases function by reducing the cellular levels of proteins and thalidomide has been shown to alter the set of proteins which CRBN can degrade.[40] Cereblon's relevance to human congenital defects was confirmed in studies that reduced the production of cereblon in developing chick and zebrafish embryos using genetic techniques. These embryos had defects similar to those treated with thalidomide. Interestingly, mice treated with thalidomide do not display teratogenicity of their offspring as seen in humans.[41]
Other actions
[edit]Thalidomide binds to and acts as an antagonist of the androgen receptor (AR).[42][43][44] In accordance, it can produce gynecomastia and sexual dysfunction as side effects in men.[45][46][47] DIMP is a non-steroidal antiandrogen which was one of the first antiandrogens to be developed, and is structurally related to thalidomide.[42][43][44]
Synthesis
[edit]Thalidomide is synthesized into a racemic mixture, however separating the mixture into a enatiomerically pure solution would prove fruitless[22][23][24] as the racemization can occur in vivo.[25][26][22][27] Celgene Corporation originally synthesized thalidomide using a three-step sequence starting with L-glutamic acid treatment, but this has since been reformed by the use of L-glutamine.[28] As shown in the image below, N-carbethoxyphtalimide (1) can react with L-glutamine to yield N-Phthaloyl-L-glutamine (2). Cyclization of N-Phthaloyl-L-glutamine occurs using carbonyldiimidazole, which then yields thalidomide (3).[28] Celegne Corporation's original method resulted in a 31% yield of S-thalidomide, whereas the two-step synthesis yields 85-93% product that is 99% pure.

References
[edit]- ^ a b c d e f Stephens TD, Bunde CJ, Fillmore BJ (June 2000). "Mechanism of action in thalidomide teratogenesis". Biochem. Pharmacol. 59 (12): 1489–99. doi:10.1016/S0006-2952(99)00388-3. PMID 10799645.
- ^ a b Stephens, T; Bunde, C; Torres, R; Hackett, D; Stark, M; Smith, D; Fillmore, B (1998). "Thalidomide inhibits limb development through its antagonism of IGF-1+ FGF-2+ heparin". Tertology. 57 (112).
{{cite journal}}:|access-date=requires|url=(help) - ^ a b Neubert, R; Hinz, N; Thiel, R; Neubert, D (15 Dec 1995). "Down-regulation of adhesion receptors on cells of primate embryos as a probable mechanism of the teratogenic action of thalidomide". Life sciences. 58 (4): 295–316.
{{cite journal}}:|access-date=requires|url=(help) - ^ a b D'Amato RJ, Loughnan MS, Flynn E, Folkman J (1994). "Thalidomide is an inhibitor of angiogenesis". Proceedings of the National Academy of Sciences of the United States of America. 91 (9): 4082–4085. Bibcode:1994PNAS...91.4082D. doi:10.1073/pnas.91.9.4082. PMC 43727. PMID 7513432.
- ^ a b Pasumarthi, Kishore B. S.; Jin, Yan; Cattini, Peter A. (18 November 2002). "Cloning of the Rat Fibroblast Growth Factor-2 Promoter Region and Its Response to Mitogenic Stimuli in Glioma C6 Cells". Journal of Neurochemistry. 68 (3): 898–908. doi:10.1046/j.1471-4159.1997.68030898.x.
- ^ a b Boisclair, Yves R.; Brown, Alexandra L.; Casola, Stefano; Rechler, Matthew M (25 Nov 1993). "Three Clustered Spl Sites Are Required for Efficient Transcription of the TATA-less Promoter of the Gene for Insulin-like Growth Factor-binding Protein-2 from the Rat". The Journal of Biological Chemistry. 268 (33): 24892–24901.
{{cite journal}}:|access-date=requires|url=(help) - ^ a b Perez-Castro, Ana V.; Wilson, Julie; Altherr, Michael R. (April 1997). "Genomic Organization of the Human Fibroblast Growth Factor Receptor 3 (FGFR3) Gene and Comparative Sequence Analysis with the MouseFgfr3Gene". Genomics. 41 (1): 10–16. doi:10.1006/geno.1997.4616.
{{cite journal}}:|access-date=requires|url=(help) - ^ a b Werner, Haim; Stannard, Bethel; Bach, Mark A.; LeRoith, Derek; Roberts, Charles T. (June 1990). "Cloning and characterization of the proximal promoter region of the rat insulin-like growth factor I (IGF-I) receptor gene". Biochemical and Biophysical Research Communications. 169 (3): 1021–1027. doi:10.1016/0006-291X(90)91996-6.
- ^ a b Cooke, David W.; Bankert, Laura A.; Roberts, Charles T.; LeRoith, Derek; Casella, Samuel J. (June 1991). "Analysis of the human type I insulin-like growth factor receptor promoter region". Biochemical and Biophysical Research Communications. 177 (3): 1113–1120. doi:10.1016/0006-291X(91)90654-P.
- ^ a b Adamo, M; Roberts CT, Jr; LeRoith, D (January 1992). "How distinct are the insulin and insulin-like growth factor I signalling systems?". BioFactors (Oxford, England). 3 (3): 151–7. PMID 1599609.
- ^ a b Myers MG, Jr; Grammer, TC; Wang, LM; Sun, XJ; Pierce, JH; Blenis, J; White, MF (18 November 1994). "Insulin receptor substrate-1 mediates phosphatidylinositol 3'-kinase and p70S6k signaling during insulin, insulin-like growth factor-1, and interleukin-4 stimulation". The Journal of biological chemistry. 269 (46): 28783–9. PMID 7961833.
- ^ a b c d Stephens, TD; Fillmore, BJ (March 2000). "Hypothesis: thalidomide embryopathy-proposed mechanism of action". Teratology. 61 (3): 189–95. PMID 10661908.
- ^ a b Therapontos, C; Erskine, L; Gardner, ER; Figg, WD; Vargesson, N (26 May 2009). "Thalidomide induces limb defects by preventing angiogenic outgrowth during early limb formation". Proceedings of the National Academy of Sciences of the United States of America. 106 (21): 8573–8. PMID 19433787.
- ^ a b Vargesson, N (June 2015). "Thalidomide-induced teratogenesis: history and mechanisms". Birth defects research. Part C, Embryo today : reviews. 105 (2): 140–56. PMID 26043938.
- ^ Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N (2010). "A meta-analysis of cytokines in Alzheimer's disease". Biol Psychiatry. 68 (10): 930–941. doi:10.1016/j.biopsych.2010.06.012. PMID 20692646.
- ^ Locksley RM, Killeen N, Lenardo MJ (2001). "The TNF and TNF receptor superfamilies: integrating mammalian biology". Cell. 104 (4): 487–501. doi:10.1016/S0092-8674(01)00237-9. PMID 11239407.
- ^ Sarno EN, Grau GE, Vieira LM, Nery JA (April 1991). "Serum levels of tumour necrosis factor-alpha and interleukin-1 beta during leprosy reactional states". Clin. Exp. Immunol. 84 (1): 103–8. doi:10.1111/j.1365-2249.1991.tb08131.x. PMC 1535359. PMID 2015700.
- ^ Moriera, Andre; Sampaio, Elizabeth; Antonina, Zmuidzinas; Paula, Frindt; Smith, Kendall; Kaplan, Gilla (1 June 1993). "Thalidomide Exerts Its Inhibitory Action on Tumor Necrosis Factor α by Enhancing mRNA Degradation". The Journal of Experimental Medicine. 177 (6): 1675–1680. doi:10.1084/jem.177.6.1675.
{{cite journal}}:|access-date=requires|url=(help) - ^ Doherty, G; Jensen, J; Alexander, H; Buresh, C; Norton, J (1 Aug 1991). "Pentoxifylline suppression of tumor necrosis factor gene transcription". Surgery. 110 (2): 192–198.
{{cite journal}}:|access-date=requires|url=(help) - ^ Han, J; Thompson, P; Beutler, B (1 Jul 1990). "Dexamethosone and penthoxifylline inhibit endotoxin-induced cachectin/tumor necrosis factor synthesis at separate points in the signaling pathway". The Journal of Experimental Medicine. 172 (1): 391–394.
{{cite journal}}:|access-date=requires|url=(help) - ^ Greig, Nigel; Girodano, Tony; Zhu, Xiaoxiang; Yu, Qian-sheng; Perry, Tracy; Holloway, Harold; Brossi, Arnold; Rogers, Jack; Sambamurti, Kumar; Lahiri, Debomoy (2004). "Thalidomide-based TNF-α inhibitors for neurodegenerative diseases". Acta neurobiologiae experimentalis. 64 (1): 1–9.
{{cite journal}}:|access-date=requires|url=(help) - ^ a b c d e f Muller GW, Corral LG, Shire MG, Wang H, Moreira A, Kaplan G, Stirling DI (August 1996). "Structural modifications of thalidomide produce analogs with enhanced tumor necrosis factor inhibitory activity". J. Med. Chem. 39 (17): 3238–40. doi:10.1021/jm9603328. PMID 8765505.
- ^ a b c Bartlett JB, Dredge K, Dalgleish AG (April 2004). "The evolution of thalidomide and its IMiD derivatives as anticancer agents". Nat. Rev. Cancer. 4 (4): 314–22. doi:10.1038/nrc1323. PMID 15057291.
- ^ a b c Man HW, Schafer P, Wong LM, Patterson RT, Corral LG, Raymon H, Blease K, Leisten J, Shirley MA, Tang Y, Babusis DM, Chen R, Stirling D, Muller GW (March 2009). "Discovery of (S)-N-[2-[1-(3-ethoxy-4-methoxyphenyl)-2-methanesulfonylethyl]-1,3-dioxo-2,3-dihydro-1H-isoindol-4-yl] acetamide (apremilast), a potent and orally active phosphodiesterase 4 and tumor necrosis factor-alpha inhibitor". J. Med. Chem. 52 (6): 1522–4. doi:10.1021/jm900210d. PMID 19256507.
- ^ a b c Cite error: The named reference
clinpwas invoked but never defined (see the help page). - ^ a b c Eriksson T, Björkman S, Roth B, Fyge A, Höglund P (1995). "Stereospecific determination, chiral inversion in vitro and pharmacokinetics in humans of the enantiomers of thalidomide". Chirality. 7 (1): 44–52. doi:10.1002/chir.530070109. PMID 7702998.
- ^ a b c Man HW, Corral LG, Stirling DI, Muller GW (October 2003). "Alpha-fluoro-substituted thalidomide analogues". Bioorg. Med. Chem. Lett. 13 (20): 3415–7. doi:10.1016/S0960-894X(03)00778-9. PMID 14505639.
- ^ a b c d Muller, George; Konnecke, William; Smith, Alison; Khetani, Vikram (19 March 1999). "A Concise Two-Step Synthesis of Thalidomide". Organic Process Research & Development. 3 (2): 139–140. doi:10.1021/op980201b. Retrieved 23 April 2017.
- ^ a b Kim, James H.; Scialli, Anthony R. (2011). "Thalidomide: The Tragedy of Birth Defects and the Effective Treatment of Disease". Toxicological Sciences. 122 (1): 1–6. doi:10.1093/toxsci/kfr088. PMID 21507989.
- ^ a b c d Singhal S, Mehta J (February 2002). "Thalidomide in cancer". Biomedicine & Pharmacotherapy. 56 (1): 4–12. doi:10.1016/S0753-3322(01)00146-9. PMID 11905508.
- ^ Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N (2010). "A meta-analysis of cytokines in Alzheimer's disease". Biol Psychiatry. 68 (10): 930–941. doi:10.1016/j.biopsych.2010.06.012. PMID 20692646.
- ^ Locksley RM, Killeen N, Lenardo MJ (2001). "The TNF and TNF receptor superfamilies: integrating mammalian biology". Cell. 104 (4): 487–501. doi:10.1016/S0092-8674(01)00237-9. PMID 11239407.
- ^ Sarno EN, Grau GE, Vieira LM, Nery JA (April 1991). "Serum levels of tumour necrosis factor-alpha and interleukin-1 beta during leprosy reactional states". Clin. Exp. Immunol. 84 (1): 103–8. doi:10.1111/j.1365-2249.1991.tb08131.x. PMC 1535359. PMID 2015700.
- ^ Moriera, Andre; Sampaio, Elizabeth; Antonina, Zmuidzinas; Paula, Frindt; Smith, Kendall; Kaplan, Gilla (1 June 1993). "Thalidomide Exerts Its Inhibitory Action on Tumor Necrosis Factor α by Enhancing mRNA Degradation". The Journal of Experimental Medicine. 177 (6): 1675–1680. doi:10.1084/jem.177.6.1675.
{{cite journal}}:|access-date=requires|url=(help) - ^ Doherty, G; Jensen, J; Alexander, H; Buresh, C; Norton, J (1 Aug 1991). "Pentoxifylline suppression of tumor necrosis factor gene transcription". Surgery. 110 (2): 192–198.
{{cite journal}}:|access-date=requires|url=(help) - ^ Han, J; Thompson, P; Beutler, B (1 Jul 1990). "Dexamethosone and penthoxifylline inhibit endotoxin-induced cachectin/tumor necrosis factor synthesis at separate points in the signaling pathway". The Journal of Experimental Medicine. 172 (1): 391–394.
{{cite journal}}:|access-date=requires|url=(help) - ^ Greig, Nigel; Girodano, Tony; Zhu, Xiaoxiang; Yu, Qian-sheng; Perry, Tracy; Holloway, Harold; Brossi, Arnold; Rogers, Jack; Sambamurti, Kumar; Lahiri, Debomoy (2004). "Thalidomide-based TNF-α inhibitors for neurodegenerative diseases". Acta neurobiologiae experimentalis. 64 (1): 1–9.
{{cite journal}}:|access-date=requires|url=(help) - ^ http://www.uniprot.org/uniprot/Q96SW2[full citation needed]
- ^ Zimmer C (March 15, 2010). "Answers Begin to Emerge on How Thalidomide Caused Defects". New York Times. Retrieved 2010-03-21.
As they report in the current issue of Science, a protein known as cereblon latched on tightly to the thalidomide
- ^ Kronke, Jan; Udeshi, Namrata D.; Narla, Anupama; Grauman, Peter; Hurst, Slater N.; McConkey, Marie; Svinkina, Tanya; Heckl, Dirk; Comer, Eamon; Li, Xiaoyu; Ciarlo, Christie; Hartman, Emily; Munshi, Nikhil; Schenone, Monica; Schreiber, Stuart L.; Carr, Steven A.; Ebert, Benjamin L. (2014). "Lenalidomide Causes Selective Degradation of IKZF1 and IKZF3 in Multiple Myeloma Cells". Science. 343 (6168): 301–5. Bibcode:2014Sci...343..301K. doi:10.1126/science.1244851. PMC 4077049. PMID 24292625.
- ^ Krönke, Jan; Fink, Emma C.; Hollenbach, Paul W.; MacBeth, Kyle J.; Hurst, Slater N.; Udeshi, Namrata D.; Chamberlain, Philip P.; Mani, D. R.; Man, Hon Wah; Gandhi, Anita K.; Svinkina, Tanya; Schneider, Rebekka K.; McConkey, Marie; Järås, Marcus; Griffiths, Elizabeth; Wetzler, Meir; Bullinger, Lars; Cathers, Brian E.; Carr, Steven A.; Chopra, Rajesh; Ebert, Benjamin L. (2015). "Lenalidomide induces ubiquitination and degradation of CK1α in del(5q) MDS". Nature. 523 (7559): 183–8. Bibcode:2015Natur.523..183K. doi:10.1038/nature14610. PMC 4853910. PMID 26131937.
- ^ a b Hashimoto, Y.; Tanatani, A.; Nagasawa, K.; Miyachi, H. (2004). "Thalidomide as a multitarget drug and its application as a template for drug design". Drugs of the Future. 29 (4): 383. doi:10.1358/dof.2004.029.04.792298. ISSN 0377-8282.
- ^ a b Liu, Bo; Su, Lei; Geng, Jingkun; Liu, Junjie; Zhao, Guisen (2010). "Developments in Nonsteroidal Antiandrogens Targeting the Androgen Receptor". ChemMedChem. 5 (10): 1651–1661. doi:10.1002/cmdc.201000259. ISSN 1860-7179.
- ^ a b Hashimoto, Yuichi (2003). "Structural development of synthetic retinoids and thalidomide-related molecules". Cancer Chemotherapy and Pharmacology. 52 (0): 16–23. doi:10.1007/s00280-003-0590-3. ISSN 0344-5704.
- ^ Ghobrial IM, Rajkumar SV (2003). "Management of thalidomide toxicity". J Support Oncol. 1 (3): 194–205. PMC 3134146. PMID 15334875.
- ^ Deepinder, Fnu; Braunstein, Glenn D (2012). "Drug-induced gynecomastia: an evidence-based review". Expert Opinion on Drug Safety. 11 (5): 779–795. doi:10.1517/14740338.2012.712109. ISSN 1474-0338. PMID 22862307.
- ^ Nuttall, Frank Q.; Warrier, Rohit S.; Gannon, Mary C. (2015). "Gynecomastia and drugs: a critical evaluation of the literature". European Journal of Clinical Pharmacology. 71 (5): 569–578. doi:10.1007/s00228-015-1835-x. ISSN 0031-6970.

