Membrane-mediated anesthesia
Membrane-mediated anesthesia or anaesthesia (UK) is a mechanism of action that involves an anesthetic agent exerting its pharmaceutical effects primarily through interaction with the lipid bilayer membrane.
The relationship between volatile (inhalable) general anesthetics and the cellular lipid membrane has been well established since around 1900, based on the Meyer-Overton Correlation.[1][2][3][4][5] Since 1900 there have been extensive research efforts to characterize these membrane-mediated effects of anesthesia, leading to many theories but few answers. During the 1980s the focus of anesthetic research shifted from membrane lipids to membrane proteins,[5][6][7] where it currently remains.[8][9][10][11] Accordingly, the specific membrane-mediated anesthetic effects remain mostly undiscovered.[9][12][13][14][15]
Recent research has demonstrated promising mechanisms of membrane-mediated anesthetic action for both general and Local anesthetics. These studies suggest that the anesthetic binding site in the membrane is within ordered lipids. This binding disrupts the function of the ordered lipids, forming lipid rafts that dislodge a membrane-bound phospholipase involved in a metabolic pathway that actives anesthetic-sensitive potassium channels.[15][16][17] Other recent studies show similar lipid-raft-specific anesthetic effects on sodium channels.[17][18]
See Theories of general anaesthetic action for a broader discussion of purely theoretical mechanisms.
The Meyer-Overton Correlation for Anesthetics
[edit]
At the turn of the twentieth century, one of the most important anesthetic-based theories began to take shape. At the time, the research of both German pharmacologist Hans Horst Meyer (1899)[1] and British-Swedish physiologist Charles Ernest Overton (1901)[2] reached the same conclusion about general anesthetics and lipids:
There is a direct correlation between anesthetic agents and lipid solubility. The more lipophillic the anesthetic agent is, the more potent the anesthetic agent is.[3][8][18]
This principle became known as the Meyer-Overton Correlation. It originally compared the anesthetic partition coefficient in olive oil (X-axis) to the effective dose that induced anesthesia in 50% (i.e., EC50) of the tadpole research subjects (Y-axis).[1][2][3][4] Modern renditions of the Meyer-Overton plot usually compare olive oil partition coefficent of the Inhalational or Intravenous drug (X-axis) to the minimum alveolar concentration (MAC) or the effective dose 50 (i.e., ED50) of the anesthetic agent (Y-axis).[citation needed]
Despite more than 175 years of anesthetic use and research, the exact connection between phospholipids, the bilayer membrane, and general anesthetic agents remains mostly unknown.[4][9][10] Accordingly, the means of membrane-mediated anesthesia remain mostly theoretical.[4][19][20]
The Lateral Pressure Profile Theory
[edit]The Lateral Pressure Profile theory suggests that anesthetic agents partition into the lipid bilayer, increasing the horizontal (lateral) pressure on proteins imbedded in the membrane. The added pressure causes a conformational change in protein structure, forcing the neuronal channel into an open or closed state (e.g., hyperpolarization) that generates the Inhibitory state of general anesthesia in the central nervous system (CNS).[20][21][citation needed]
This is the first hypothesis to explain the correlations of anesthetic potency with lipid bilayer structural characteristics, describing both mechanistic and thermodynamic rationale for the effects of general anesthesia.[citation needed]
General anesthetics
[edit]Inhaled anesthetics partition into the membrane and disrupt the function of ordered lipids.[15] Membranes, like proteins, are composed of ordered and disordered regions.[14] The ordered region of the membrane contains a palmitate binding site that drives the association of palmitoylated proteins to clusters of GM1 lipids (sometimes referred to as lipid rafts). Palmitate's binding to lipid rafts regulates the affinity of most proteins to lipid rafts.[22]
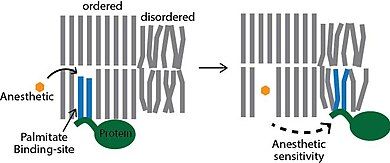
Inhaled anesthetics partition into the lipid membrane and disrupt the binding of palmitate to GM1 lipids (see figure). The anesthetic binds to a specific palmitate site nonspecifically. The clusters of GM1 lipids persist, but they lose their ability to bind palmitoylated proteins.[23]
PLD2
[edit]Phospholipase D2 (PLD2) is a palmitoylated protein that is activated by substrate presentation.[24] Anesthetics cause PLD2 to move from GM1 lipids, where it lacks access to its substrate, to a PIP2 domain which has abundant PLD2 substrate.[23] Animals with genetically depleted PLD2 were significantly resistant to anesthetics. The anesthetics xenon, chloroform, isofluorane, and propofol all activate PLD in cultured cells.
TREK-1
[edit]Twik-related potassium channel (TREK-1) is localized to ordered lipids through its interaction with PLD2. Displacement of the complex from GM1 lipids causes the complex to move to clusters. The product of PLD2, phosphatidic acid (PA) directly activates TREK-1.[25] The anesthetic sensitivity of TREK-1 was shown to be through PLD2, and the sensitivity could be transferred to TRAAK, an otherwise anesthetic insensitive channel.[15]
GABAAR
[edit]The membrane mediated mechanism is still being investigated. Nonetheless, the GABAAR gamma subunit is palmitoylated and the alpha subunit binds to PIP2. When the agonist GABA binds to GABAAR it causes a translocation to thin lipids near PIP2.[26] Anesthetic disruption of Palmitate mediated localization should therefore cause the channel to move the same as an agonist, but this has not yet been confirmed.
Endocytosis
[edit]Endocytosis helps regulate the time an ion channel spends on the surface of the membrane. GM1 lipids are the site of endocytosis. The anesthetics hydroxychloroquine, tetracaine, and lidocaine blocked entry of palmitoylated protein into the endocytic pathway.[27] By blocking access to GM1 lipids, anesthetics block access to endocytosis through a membrane-mediated mechanism.
Local anesthetics
[edit]Local anesthetics disrupt ordered lipid domains and this can cause PLD2 to leave a lipid raft.[16] They also disrupt protein interactions with PIP2.[27]
History
[edit]More than 100 years ago, a unifying theory of anesthesia was proposed based on the oil partition coefficient. In the 70s this concept was extended to the disruption of lipid partitioning.[28] Partitioning itself is an integral part of forming the ordered domains in the membrane, and the proposed mechanism is very close to the current thinking, but the partitioning itself is not the target of the anesthetics. At clinical concentration, the anesthetics do not inhibit lipid partitioning.[15] Rather they inhibit the order within the partition and/or compete for the palmitate binding site. Nonetheless, several of the early conceptual ideas about how disruption of lipid partitioning could affect an ion channel have merit.
References
[edit]- ^ a b c Meyer, Hans (1899-03-01). "Zur Theorie der Alkoholnarkose". Archiv für experimentelle Pathologie und Pharmakologie (in German). 42 (2): 109–118. doi:10.1007/BF01834479. ISSN 1432-1912.
- ^ a b c Overton, Charles Ernest (1901). Studien über die Narkose: zugleich ein Beitrag zur allgemeinen Pharmakologie (in German). G. Fischer.
- ^ a b c Missner, Andreas; Pohl, Peter (2009). "110 Years of the Meyer–Overton Rule: Predicting Membrane Permeability of Gases and Other Small Compounds". ChemPhysChem. 10 (9–10): 1405–1414. doi:10.1002/cphc.200900270. ISSN 1439-7641. PMC 3045804. PMID 19514034.
- ^ a b c d Lynch, Carl III (2008). "Meyer and Overton Revisited". Anesthesia & Analgesia. 107 (3): 864–867. doi:10.1213/ane.0b013e3181706c7e. ISSN 0003-2999.
- ^ a b Bean, B P; Shrager, P; Goldstein, D A (1981-03-01). "Modification of sodium and potassium channel gating kinetics by ether and halothane". Journal of General Physiology. 77 (3): 233–253. doi:10.1085/jgp.77.3.233. ISSN 0022-1295. PMC 2215432. PMID 6265590.
- ^ Franks, N. P.; Lieb, W. R. (1984). "Do general anaesthetics act by competitive binding to specific receptors?". Nature. 310 (5978): 599–601. Bibcode:1984Natur.310..599F. doi:10.1038/310599a0. ISSN 1476-4687. PMID 6462249.
- ^ Bovill, James G. (2000). "Mechanisms of anaesthesia: time to say farewell to the Meyer-Overton rule". Current Opinion in Anesthesiology. 13 (4): 433–436. doi:10.1097/00001503-200008000-00006. ISSN 0952-7907. PMID 17016337.
- ^ a b Clayton, Thomas; Ode, Kenichi (2023-04-01). "Mechanisms of action of general anaesthetic drugs". Anaesthesia & Intensive Care Medicine. 24 (4): 235–237. doi:10.1016/j.mpaic.2022.12.031. ISSN 1472-0299.
- ^ a b c Reigada, Ramon (2013-01-02). "Atomistic Study of Lipid Membranes Containing Chloroform: Looking for a Lipid-Mediated Mechanism of Anesthesia". PLOS ONE. 8 (1): e52631. Bibcode:2013PLoSO...852631R. doi:10.1371/journal.pone.0052631. ISSN 1932-6203. PMC 3534722. PMID 23300982.
- ^ a b Hao, Xuechao; Ou, Mengchan; Zhang, Donghang; Zhao, Wenling; Yang, Yaoxin; Liu, Jin; Yang, Hui; Zhu, Tao; Li, Yu; Zhou, Cheng (2020). "The Effects of General Anesthetics on Synaptic Transmission". Current Neuropharmacology. 18 (10): 936–965. doi:10.2174/1570159X18666200227125854. PMC 7709148. PMID 32106800.
- ^ Franks, Nicholas P (2006). "Molecular targets underlying general anaesthesia". British Journal of Pharmacology. 147 (S1): S72–S81. doi:10.1038/sj.bjp.0706441. ISSN 1476-5381. PMC 1760740. PMID 16402123.
- ^ Antkowiak, Bernd (2001-05-01). "How do general anaesthetics work?". Naturwissenschaften. 88 (5): 201–213. Bibcode:2001NW.....88..201A. doi:10.1007/s001140100230. ISSN 1432-1904. PMID 11482433.
- ^ Ramírez, Carlos (2022-03-07). "Lipids, Chloroform, and Their Intertwined Histories". Substantia. 6 (1): 133–143. doi:10.36253/Substantia-1498. ISSN 2532-3997.
- ^ a b Sezgin, Erdinc; Levental, Ilya; Mayor, Satyajit; Eggeling, Christian (2017). "The mystery of membrane organization: composition, regulation and roles of lipid rafts". Nature Reviews Molecular Cell Biology. 18 (6): 361–374. doi:10.1038/nrm.2017.16. ISSN 1471-0080. PMC 5500228. PMID 28356571.
- ^ a b c d e Pavel, MA; Petersen, EN; Wang, H; Lerner, RA; Hansen, SB (16 June 2020). "Studies on the mechanism of general anesthesia". Proceedings of the National Academy of Sciences of the United States of America. 117 (24): 13757–13766. Bibcode:2020PNAS..11713757P. doi:10.1073/pnas.2004259117. PMC 7306821. PMID 32467161.
- ^ a b Pavel, MA; Chung, HW; Petersen, EN; Hansen, SB (October 2019). "Polymodal Mechanism for TWIK-Related K+ Channel Inhibition by Local Anesthetic". Anesthesia and Analgesia. 129 (4): 973–982. doi:10.1213/ANE.0000000000004216. PMID 31124840. S2CID 163166750.
- ^ a b Krogman, William L.; Woodard, Thomas; McKay, Robert S. F. (2024). "Anesthetic Mechanisms: Synergistic Interactions With Lipid Rafts and Voltage-Gated Sodium Channels". Anesthesia & Analgesia. 139 (1): 92–106. doi:10.1213/ANE.0000000000006738. ISSN 0003-2999. PMID 37968836.
- ^ a b Baskerville, Charles (1911-08-11). "The Chemistry of Anesthetics". Science. 34 (867): 161–176. Bibcode:1911Sci....34..161B. doi:10.1126/science.34.867.161. PMID 17814438.
- ^ Brown, Emery N.; Pavone, Kara J.; Naranjo, Marusa (November 2018). "Multimodal General Anesthesia: Theory and Practice". Anesthesia & Analgesia. 127 (5): 1246–1258. doi:10.1213/ANE.0000000000003668. ISSN 0003-2999. PMC 6203428. PMID 30252709.
- ^ a b Cantor, Robert S. (1997-03-01). "The Lateral Pressure Profile in Membranes: A Physical Mechanism of General Anesthesia". Biochemistry. 36 (9): 2339–2344. doi:10.1021/bi9627323. ISSN 0006-2960. PMID 9054538.
- ^ Cantor, Robert S (1998-11-23). "The lateral pressure profile in membranes: a physical mechanism of general anesthesia". Toxicology Letters. 100–101: 451–458. doi:10.1016/S0378-4274(98)00220-3. ISSN 0378-4274. PMID 10049179.
- ^ Levental, I; Lingwood, D; Grzybek, M; Coskun, U; Simons, K (21 December 2010). "Palmitoylation regulates raft affinity for the majority of integral raft proteins". Proceedings of the National Academy of Sciences of the United States of America. 107 (51): 22050–4. Bibcode:2010PNAS..10722050L. doi:10.1073/pnas.1016184107. PMC 3009825. PMID 21131568.
- ^ a b Petersen, EN; Pavel, MA; Wang, H; Hansen, SB (1 January 2020). "Disruption of palmitate-mediated localization; a shared pathway of force and anesthetic activation of TREK-1 channels". Biochimica et Biophysica Acta (BBA) - Biomembranes. 1862 (1): 183091. doi:10.1016/j.bbamem.2019.183091. PMC 6907892. PMID 31672538.
- ^ Petersen, EN; Chung, HW; Nayebosadri, A; Hansen, SB (15 December 2016). "Kinetic disruption of lipid rafts is a mechanosensor for phospholipase D." Nature Communications. 7: 13873. Bibcode:2016NatCo...713873P. doi:10.1038/ncomms13873. PMC 5171650. PMID 27976674.
- ^ Comoglio, Y; Levitz, J; Kienzler, MA; Lesage, F; Isacoff, EY; Sandoz, G (16 September 2014). "Phospholipase D2 specifically regulates TREK potassium channels via direct interaction and local production of phosphatidic acid". Proceedings of the National Academy of Sciences of the United States of America. 111 (37): 13547–52. Bibcode:2014PNAS..11113547C. doi:10.1073/pnas.1407160111. PMC 4169921. PMID 25197053.
- ^ Yuan, Zixuan; Pavel, Mahmud Arif; Hansen, Scott B. (29 April 2024), "GABA and astrocytic cholesterol determine the lipid environment of GABA A R in cultured cortical neurons", bioRxiv: 2024.04.26.591395, doi:10.1101/2024.04.26.591395, PMC 11092523, PMID 38746110
- ^ a b Yuan, Z; Pavel, MA; Wang, H; Kwachukwu, JC; Mediouni, S; Jablonski, JA; Nettles, KW; Reddy, CB; Valente, ST; Hansen, SB (14 September 2022). "Hydroxychloroquine blocks SARS-CoV-2 entry into the endocytic pathway in mammalian cell culture". Communications Biology. 5 (1): 958. doi:10.1038/s42003-022-03841-8. PMC 9472185. PMID 36104427.
- ^ Trudell, JR (January 1977). "A unitary theory of anesthesia based on lateral phase separations in nerve membranes". Anesthesiology. 46 (1): 5–10. doi:10.1097/00000542-197701000-00003. PMID 12686. S2CID 24107213.
