Ondansetron
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Zofran, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601209 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, rectal, intravenous, intramuscular, thin film |
| Drug class | |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~60% |
| Protein binding | 70–76% |
| Metabolism | Liver (CYP3A4, CYP1A2, CYP2D6) |
| Elimination half-life | 5.7 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.110.918 |
| Chemical and physical data | |
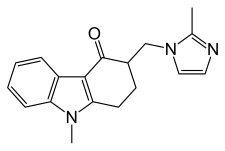
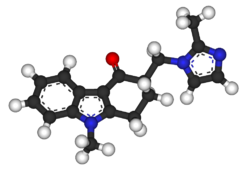
| Formula | C18H19N3O |
| Molar mass | 293.370 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Ondansetron, sold under the brand name Zofran among others, is a medication used to prevent nausea and vomiting caused by chemotherapy, radiation therapy, migraines, or surgery.[8] It is also effective for treating gastroenteritis.[9][10] It can be given orally (by mouth), intramuscularly (injection into a muscle), or intravenously (injection into a vein).[8]
Common side effects include diarrhea, constipation, headache, sleepiness, and itchiness.[8] Serious side effects include QT prolongation and severe allergic reaction.[8] It appears to be safe during pregnancy but has not been well studied in this group.[8] It is a serotonin 5-HT3 receptor antagonist.[8] It does not have any effect on dopamine receptors or muscarinic acetylcholine receptors.[11]
Ondansetron was patented in 1984 and approved for medical use in 1990.[12] It is on the World Health Organization's List of Essential Medicines.[13] It is available as a generic medication.[8] In 2022, it was the 61st most commonly prescribed medication in the United States, with more than 10 million prescriptions.[14][15]
Medical uses
[edit]Ondansetron is indicated for the prevention of chemotherapy-induced nausea and vomiting and postoperative nausea and vomiting.[6][16]
Pregnancy
[edit]Ondansetron is used off-label to treat morning sickness and hyperemesis gravidarum of pregnancy. It is typically used after other antiemetic drugs have failed.[17]
A large multi-center cohort study found no association between ondansetron exposure and fetal risk compared to other antiemetics.[18]
Cyclic vomiting syndrome
[edit]Ondansetron is one of several antiemetics used during the vomiting phase of cyclic vomiting syndrome.[19]
Gastroenteritis
[edit]Trials in emergency department settings support the use of ondansetron to abort vomiting episodes associated with gastroenteritis and dehydration.[20] A randomized controlled trial using a single dose of oral ondansetron in children with presumably viral gastroenteritis found it to be highly effective in stopping vomiting and increasing the effectiveness of oral rehydration therapy, thereby significantly increasing patient satisfaction. Only 16 of the 123 children treated with ondansetron vomited in the following 6 hours.[21] A retrospective review found that ondansetron was used commonly for vomiting due to gastroenteritis, being administered in over 58% of cases. Its use reduced hospital admissions, but was also associated with higher rates of return visits to the emergency department. Furthermore, people who had initially received ondansetron were more likely to be admitted on the return visit than people who had not received the drug. However, this effect may simply be due to the agent being used more frequently in people who present with more severe illness. Its use was not found to mask serious diagnoses.[22]
Irritable bowel syndrome (IBS)
[edit]In a study of patients diagnosed as having IBS with diarrhea (IBS-D), ondansetron showed statistically significant effects on stool consistency, frequency, urgency and bloating, but not on pain scores.[23] This was confirmed in a later trial and meta-analysis[24] and is included in international guidelines.[25]
Special populations
[edit]Children
[edit]Ondansetron has rarely been studied in people under 4 years of age. As such, little data is available to guide dosage recommendations.[6]
Three open non-comparative studies have been conducted to assess the safety and efficacy of ondansetron in children receiving a variety of chemotherapy regimens.[26]
Ondansetron was well tolerated and none of the patients experienced extrapyramidal symptoms.[27]
Adverse effects
[edit]Headache is the most common adverse effect.[6] A review of use for post-operative nausea and vomiting found that for every 36 people treated, one would experience headache, which could be severe.[28]
Constipation, diarrhea, and dizziness are other commonly reported side effects. It is broken down by the hepatic cytochrome P450 system and it has little effect on the metabolism of other drugs broken down by this system.[8]
QT prolongation
[edit]Use of ondansetron has been associated with prolongation of the QT interval, which can lead to a potentially fatal heart rhythm known as torsades de pointes. Although this may happen in any person with any formulation, the risk is most salient with the injectable (intravenous) form of the drug and increases with dose. The risk is also higher in people taking other medicines that prolong the QT interval, as well as in people with congenital long QT syndrome, congestive heart failure, and/or bradyarrhythmias. As such, single doses of injectable ondansetron should not exceed 16 mg at one time. (Oral dosing recommendations remain intact, including the recommendation of a single 24 mg oral dose when indicated.) Electrolyte imbalances should be corrected before the use of injectable ondansetron. People are cautioned to seek immediate medical care if symptoms such as irregular heartbeat/palpitations, shortness of breath, dizziness, or fainting occur while taking ondansetron.[29]
Overdose
[edit]No specific treatment is available for ondansetron overdose; people are managed with supportive measures. An antidote to ondansetron is not known.[6]
Pharmacology
[edit]Pharmacodynamics
[edit]Ondansetron is a highly selective serotonin 5-HT3 receptor antagonist, with low affinity for dopamine receptors. The 5-HT3 receptors are present both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema in the medulla. Serotonin is released by the enterochromaffin cells of the small intestine in response to chemotherapeutic agents and may stimulate vagal afferents (via 5-HT3 receptors) to initiate the vomiting reflex. It is thought that ondansetron's antiemetic action is mediated mostly via antagonism of vagal afferents with a minor contribution from antagonism of central receptors.[30] The R– and S–ondansetron isomers have similar potency as serotonin antagonists when tested on ex vivo rat vagus nerve.[31] However, the R–ondansetron enantiomer was 7.9 times more potent as an antagonist of serotonin and 2-methyl-5-hydroxytryptamine (2-methylserotonin) when tested on the longitudinal smooth muscle from guinea pig ileum. However, the guinea pig ileum test was likely not as faithful as a test of 5-HT3 receptor antagonism, because ondansetron only partially blocked the effect of serotonin, while it completely blocked the effect of 2-methylserotonin.[31]
Pharmacokinetics
[edit]Ondansetron may have a degree of peripheral selectivity due to binding to P-glycoprotein and efflux out of the brain at the blood–brain barrier.[32][33][34] Ondansetron is marketed as a racemic mixture of R–(–)–ondansetron and S–(+)–ondansetron, and the two enantiomers have significantly different kinetics. In rats given 2 mg/kg intravenous doses of each enantiomer separately, R–(–)–ondansetron was found to have a 37% longer half-life (P < 0.05) and an 87% higher area-under-curve or AUC (P < 0.01) compared to S–(+)–ondansetron, indicating that the R enantiomer is metabolized more slowly.[35] The chiral carbon in ondansetron is adjacent to a carbonyl group, so keto-enol tautomerism could theoretically lead to interconversion between the two enantiomers under physiologic conditions, if the hydrogen on the chiral carbon were removed and then replaced with opposite chirality. An experiment in rats given each enantiomer separately showed no evidence of this interconversion, the chirality was stable in vivo.[35] A study of 141 human patients given 4 or 8 mg of intravenous ondansetron for the prevention of post-operative nausea and vomiting also found that R and S–ondansetron have different pharmacokinetic properties. Each patient was classified according to their genotype for the liver enzymes CYP2D6 and CYP3A5, and they were put on a spectrum between poor metabolizers (slow) and ultra metabolizers (fast). CYP2D6 was found to be more important for the elimination of S–ondansetron, whereas CYP3A5 genotype had no impact on S–ondansetron plasma levels, measured 3 hours after drug administration. CYP3A5 was more important for R–ondansetron clearance, and CYP2D6 genotype had no consistent effect on plasma levels of R–ondansetron at 3 hours.[36]
History
[edit]
Ondansetron (marketed under the brand name Zofran) was developed in the mid-1980s by GlaxoSmithKline in London. It was granted U.S. patent protection in September 1987,[37] received a use patent June 1988,[38] and was approved by the U.S. Food and Drug Administration (FDA) in January 1991. It was granted another divisional patent in November 1996.[39] Finally, owing to GlaxoSmithKline's research on pediatric use, ondansetron's patent protection was extended until December 2006.[40] By this final year of its patent (2006), Zofran had become the 20th highest-selling brand-name drug in the United States, with sales of US$1.3 billion in the first 9 months of 2006 (80% from the US).[41] The first generic versions were approved by the U.S. FDA in December 2006, with marketing approval granted to Teva Pharmaceuticals USA and SICOR Pharmaceuticals.[42]
In December 2012, the FDA announced that the 32 mg, single intravenous (IV) dose of ondansetron was being withdrawn from U.S. market because of the potential for serious cardiac issues from prolonged QT interval.[43]
In 2018, University of São Paulo and Biolab were granted a patent for an orodispersible form of the drug.[44]
Society and culture
[edit]Publication bias
[edit]In 1997, ondansetron was the subject of a meta-analysis case study. Researchers examined 84 trials, with 11,980 people receiving ondansetron, published between 1991 and September 1996. Intravenous ondansetron 4 mg versus placebo was investigated in 16 reports and three further reports which had been duplicated a total of six times. The number needed to treat (NNT) to prevent vomiting within 24 hours was 9.5, with 95% confidence interval 6.9 to 15, in the 16 nonduplicated reports. In the three duplicated reports, the NNT was significantly lower at 3.9 (3.3 to 4.8). When all 25 reports were combined, the apparent NNT improved to 4.9 (4.4 to 5.6). Inclusion of duplicate reports led to a 23% overestimation of ondansetron's antiemetic efficacy.[45]
In addition, the authors found the covert duplication of reports on ondansetron was not easy to detect, because of lack of cross-referencing between papers, and reports containing duplicate findings were cited in eight reviews of the drug.[45] Their analysis was a subject of an editorial in the Journal of the American Medical Association in 1999.[46]
Availability
[edit]Ondansetron is a generic medication and is available in many countries under many brand names.[1]
References
[edit]- ^ a b "Ondansetron international". Drugs.com. 2 September 2020. Archived from the original on 21 February 2014. Retrieved 2 February 2014.
- ^ "Ondansetron Use During Pregnancy". Drugs.com. 3 October 2019. Archived from the original on 18 September 2020. Retrieved 7 September 2020.
- ^ "Zofran Product and Consumer Medicine Information Licence". TGA eBS. Archived from the original on 29 August 2022. Retrieved 28 August 2022.
- ^ "Zofran Product information". Health Canada. 25 April 2012. Archived from the original on 29 August 2022. Retrieved 28 August 2022.
- ^ "Zofran Tablets 4 mg - Summary of Product Characteristics (SmPC)". (emc). 19 January 2022. Archived from the original on 29 August 2022. Retrieved 28 August 2022.
- ^ a b c d e "Zofran- ondansetron hydrochloride tablet, film coated". DailyMed. 24 June 2020. Archived from the original on 6 August 2020. Retrieved 7 September 2020.
- ^ "List of nationally authorised medicinal products : Active substance: ondansetron :Procedure no.: PSUSA/00002217/202102" (PDF). Ema.europa.eu. Retrieved 5 March 2022.
- ^ a b c d e f g h "Ondansetron Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 3 May 2016. Retrieved 11 February 2017.
- ^ Schnadower D, Finkelstein Y, Freedman SB (January 2015). "Ondansetron and probiotics in the management of pediatric acute gastroenteritis in developed countries". Current Opinion in Gastroenterology. 31 (1): 1–6. doi:10.1097/mog.0000000000000132. PMID 25333367. S2CID 9334264.
- ^ Freedman SB, Ali S, Oleszczuk M, Gouin S, Hartling L (July 2013). "Treatment of acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries". Evidence-Based Child Health. 8 (4): 1123–37. doi:10.1002/ebch.1932. PMID 23877938.
- ^ Miloro M, ed. (2012). Peterson's principles of oral and maxillofacial surgery (3rd ed.). Shelton, CT: People's Medical Pub. House-USA. p. 86. ISBN 978-1-60795-111-7. Archived from the original on 1 February 2016.
- ^ FischerJ, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 448. ISBN 9783527607495. Archived from the original on 12 January 2023. Retrieved 25 August 2020.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Ondansetron Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ "Ondansetron hydrochloride injection". DailyMed. 19 October 2022. Archived from the original on 8 July 2023. Retrieved 8 July 2023.
- ^ Smith JA, Refuerzo JS, Ramin SM. "Treatment and outcome of nausea and vomiting of pregnancy". UpToDate. Archived from the original on 3 December 2013.
- ^ Dormuth CR, Winquist B, Fisher A, et al. (April 2021). "Comparison of Pregnancy Outcomes of Patients Treated With Ondansetron vs Alternative Antiemetic Medications in a Multinational, Population-Based Cohort". JAMA Netw Open. 4 (4): e215329. doi:10.1001/jamanetworkopen.2021.5329. PMC 8065380. PMID 33890993.
- ^ Abell TL, Adams KA, Boles RG, Bousvaros A, Chong SK, Fleisher DR, et al. (April 2008). "Cyclic vomiting syndrome in adults" (PDF). Neurogastroenterology and Motility. 20 (4): 269–84. doi:10.1111/j.1365-2982.2008.01113.x. hdl:2027.42/72300. PMID 18371009. S2CID 8718836. Archived from the original on 28 August 2021. Retrieved 4 November 2018.
- ^ Freedman SB, Adler M, Seshadri R, Powell EC (April 2006). "Oral ondansetron for gastroenteritis in a pediatric emergency department". The New England Journal of Medicine. 354 (16): 1698–705. doi:10.1056/NEJMoa055119. PMID 16625009. S2CID 13712069.
- ^ Hanif H, Jaffry H, Jamshed F, Amreek F, Kumar N, Hussain W, et al. (September 2019). "Oral Ondansetron versus Domperidone for Acute Gastroenteritis Associated Vomiting in Young Children". Cureus. 11 (9): e5639. doi:10.7759/cureus.5639. PMC 6822884. PMID 31700742.
- ^ Sturm JJ, Hirsh DA, Schweickert A, Massey R, Simon HK (May 2010). "Ondansetron use in the pediatric emergency department and effects on hospitalization and return rates: are we masking alternative diagnoses?". Annals of Emergency Medicine. 55 (5): 415–22. doi:10.1016/j.annemergmed.2009.11.011. PMID 20031265.
- ^ Garsed K, Chernova J, Hastings M, Lam C, Marciani L, Singh G, et al. (October 2014). "A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea". Gut. 63 (10): 1617–1625. doi:10.1136/gutjnl-2013-305989. PMC 4173656. PMID 24334242.
- ^ Gunn D, Topan R, Barnard L, Fried R, Holloway I, Brindle R, et al. (June 2023). "Randomised, placebo-controlled trial and meta-analysis show benefit of ondansetron for irritable bowel syndrome with diarrhoea: The TRITON trial". Alimentary Pharmacology & Therapeutics. 57 (11): 1258–1271. doi:10.1111/apt.17426. PMID 36866724.
- ^ Savarino E, Zingone F, Barberio B, Marasco G, Akyuz F, Akpinar H, et al. (July 2022). "Functional bowel disorders with diarrhoea: Clinical guidelines of the United European Gastroenterology and European Society for Neurogastroenterology and Motility". United European Gastroenterology Journal. 10 (6): 556–584. doi:10.1002/ueg2.12259. PMC 9278595. PMID 35695704.
- ^ Stevens RF (1 January 1991). "The role of ondansetron in paediatric patients: a review of three studies". European Journal of Cancer. 27 (Suppl 1): S20 – S22. PMID 1831631. Archived from the original on 8 July 2023. Retrieved 8 July 2023.
- ^ Stevens RF (1 January 1991). "The role of ondansetron in paediatric patients: a review of three studies". European Journal of Cancer. 27 (Suppl 1): S20 – S22. PMID 1831631. Archived from the original on 8 July 2023. Retrieved 8 July 2023.
- ^ Tramèr MR, Reynolds DJ, Moore RA, McQuay HJ (December 1997). "Efficacy, dose-response, and safety of ondansetron in prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized placebo-controlled trials". Anesthesiology. 87 (6): 1277–89. doi:10.1097/00000542-199712000-00004. PMID 9416710. S2CID 8049193.
- ^ "FDA Drug Safety Communication: New information regarding QT prolongation with ondansetron (Zofran)". Food and Drug Administration. Archived from the original on 14 December 2012. Retrieved 29 November 2012.
- ^ Browning KN (October 2015). "Role of central vagal 5-HT3 receptors in gastrointestinal physiology and pathophysiology". Frontiers in Neuroscience. 9: 413. doi:10.3389/fnins.2015.00413. PMC 4625078. PMID 26578870.
- ^ a b Butler A, Hill JM, Ireland SJ, Jordan CC, Tyers MB (June 1988). "Pharmacological properties of GR38032F, a novel antagonist at 5-HT3 receptors". British Journal of Pharmacology. 94 (2): 397–412. doi:10.1111/j.1476-5381.1988.tb11542.x. PMC 1854010. PMID 2969267.
- ^ Schinkel AH, Wagenaar E, Mol CA, van Deemter L (June 1996). "P-glycoprotein in the blood-brain barrier of mice influences the brain penetration and pharmacological activity of many drugs". Journal of Clinical Investigation. 97 (11): 2517–24. doi:10.1172/JCI118699. PMC 507337. PMID 8647944.
- ^ Kwan C, Bédard D, Frouni I, Gaudette F, Beaudry F, Hamadjida A, et al. (July 2020). "Pharmacokinetic profile of the selective 5-HT3 receptor antagonist ondansetron in the rat: an original study and a minireview of the behavioural pharmacological literature in the rat". Canadian Journal of Physiology and Pharmacology. 98 (7): 431–440. doi:10.1139/cjpp-2019-0551. PMID 32017606. S2CID 211035717.
- ^ Scott JA, Wood M, Flood P (September 2006). "The pronociceptive effect of ondansetron in the setting of P-glycoprotein inhibition". Anesthesia & Analgesia. 103 (3): 742–6. doi:10.1213/01.ane.0000228861.80314.22. PMID 16931690. S2CID 44405604.
- ^ a b Duan M, Zhao Q, Zhong D, Yuan Y (March 2019). "Pharmacokinetics of R-(-)ondansetron compared with that of S-(-)ondansetron in rats using an LC-MS/MS method". Biomedical Chromatography. 33 (3): e4426. doi:10.1002/bmc.4426. PMID 30408206.
- ^ Stamer UM, Lee EH, Rauers NI, Zhang L, Kleine-Brueggeney M, Fimmers R, et al. (July 2011). "CYP2D6- and CYP3A-dependent enantioselective plasma concentrations of ondansetron in postanesthesia care". Anesthesia and Analgesia. 113 (1): 48–54. doi:10.1213/ANE.0b013e31821d01bc. PMID 21596874.
- ^ US patent 4695578, Coates IH, Bell JA, Humber DC, Ewan GB, "1,2,3,9-tetrahydro-3-imidazol-1-ylmethyl-4H-carbazol-4-ones, composition containing them, and method of using them to treat neuronal 5HT function disturbances", issued 22 September 1987, assigned to Glaxo Group Limited
- ^ US patent 4753789, Tyers MB, Coates IH, Humber DC, Ewan GB, Bell JA, "Method for treating nausea and vomiting", issued 28 June 1988, assigned to Glaxo Group Limited
- ^ US patent 5578628, Tyers MB, Coates IH, Humber DC, Ewan GB, Bell JA, "Medicaments for the treatment of nausea and vomiting", issued 26 November 1996, assigned to Glaxo Group Limited
- ^ "One Year Post-Pediatric Exclusivity Post-marketing Adverse Event Review: Drug Use Data Zofran" (PDF). Memorandum. U.S. Food and Drug Administration. 7 March 2006. Archived (PDF) from the original on 24 September 2015.
- ^ IHS. (2006). Generics firms line up to enter Zofran market. Retrieved from "Generics Firms Line Up to Enter Zofran Market". Archived from the original on 1 February 2014. Retrieved 20 January 2014.
- ^ "FDA Approves First Generic Ondansetron Tablets, Orally Disintegrating Tablets and Oral Solution" (Press release). U.S. Food and Drug Administration. 17 December 2006. Archived from the original on 18 June 2014.
- ^ "FDA Drug Safety Communication: Updated information on 32 mg intravenous ondansetron (Zofran) dose and pre-mixed ondansetron products". U.S. Food and Drug Administration (FDA). Archived from the original on 13 December 2019. Retrieved 12 December 2012.
- ^ "Sabia que um remédio para enjoo traz 90% dos royalties que a USP recebe? - Agência USP de Inovação" (in Brazilian Portuguese). Retrieved 6 October 2020.
- ^ a b Tramèr MR, Reynolds DJ, Moore RA, McQuay HJ (September 1997). "Impact of covert duplicate publication on meta-analysis: a case study". BMJ. 315 (7109): 635–40. doi:10.1136/bmj.315.7109.635. PMC 2127450. PMID 9310564.
- ^ Rennie D (November 1999). "Fair conduct and fair reporting of clinical trials". JAMA. 282 (18): 1766–8. doi:10.1001/jama.282.18.1766. PMID 10568651.
