Synthetic lethality
Synthetic lethality is defined as a type of genetic interaction where the combination of two genetic events results in cell death or death of an organism.[1] Although the foregoing explanation is wider than this, it is common when referring to synthetic lethality to mean the situation arising by virtue of a combination of deficiencies of two or more genes leading to cell death (whether by means of apoptosis or otherwise), whereas a deficiency of only one of these genes does not. In a synthetic lethal genetic screen, it is necessary to begin with a mutation that does not result in cell death, although the effect of that mutation could result in a differing phenotype (slow growth for example), and then systematically test other mutations at additional loci to determine which, in combination with the first mutation, causes cell death arising by way of deficiency or abolition of expression.
Synthetic lethality has utility for purposes of molecular targeted cancer therapy. The first example of a molecular targeted therapeutic agent, which exploited a synthetic lethal approach, arose by means of an inactivated tumor suppressor gene (BRCA1 and 2), a treatment which received FDA approval in 2016 (PARP inhibitor).[2] A sub-case of synthetic lethality, where vulnerabilities are exposed by the deletion of passenger genes rather than tumor suppressor is the so-called "collateral lethality".[3]
Background
[edit]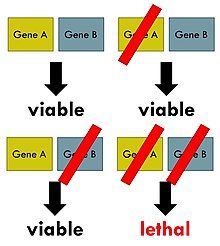
The phenomenon of synthetic lethality was first described by Calvin Bridges in 1922, who noticed that some combinations of mutations in the model organism Drosophila melanogaster (the common fruit fly) confer lethality.[1] Theodore Dobzhansky coined the term "synthetic lethality" in 1946 to describe the same type of genetic interaction in wildtype populations of Drosophila.[4] If the combination of genetic events results in a non-lethal reduction in fitness, the interaction is called synthetic sickness. Although in classical genetics the term synthetic lethality refers to the interaction between two genetic perturbations, synthetic lethality can also apply to cases in which the combination of a mutation and the action of a chemical compound causes lethality, whereas the mutation or compound alone are non-lethal.[5]
Synthetic lethality is a consequence of the tendency of organisms to maintain buffering schemes (i.e. backup plans) which engender phenotypic stability notwithstanding underlying genetic variations, environmental changes or other random events, such as mutations. This genetic robustness is the result of parallel redundant pathways and "capacitor" proteins that camouflage the effects of mutations so that important cellular processes do not depend on any individual component.[6] Synthetic lethality can help identify these buffering relationships, and what type of disease or malfunction that may occur when these relationships break down, through the identification of gene interactions that function in either the same biochemical process or pathways that appear to be unrelated.[7]
High-throughput screens
[edit]High-throughput synthetic lethal screens may help illuminate questions about how cellular processes work without previous knowledge of gene function or interaction. Screening strategy must take into account the organism used for screening, the mode of genetic perturbation, and whether the screen is forward or reverse. Many of the first synthetic lethal screens were performed in Saccharomyces cerevisiae. Budding yeast has many experimental advantages in screens, including a small genome, fast doubling time, both haploid and diploid states, and ease of genetic manipulation.[8] Gene ablation can be performed using a PCR-based strategy and complete libraries of knockout collections for all annotated yeast genes are publicly available. Synthetic genetic array (SGA), synthetic lethality by microarray (SLAM), and genetic interaction mapping (GIM) are three high-throughput methods for analyzing synthetic lethality in yeast. A genome scale genetic interaction map was created by SGA analysis in S. cerevisiae that comprises about 75% of all yeast genes.[9]
Collateral lethality
[edit]Collateral lethality is a sub-case of synthetic lethality in personalized cancer therapy, where vulnerabilities are exposed by the deletion of passenger genes rather than tumor suppressor genes, which are deleted by virtue of chromosomal proximity to major deleted tumor suppressor loci.[3]
DDR deficiencies
[edit]DNA mismatch repair deficiency
[edit]Mutations in genes employed in DNA mismatch repair (MMR) cause a high mutation rate.[10][11] In tumors, such frequent subsequent mutations often generate "non-self" immunogenic antigens. A human Phase II clinical trial, with 41 patients, evaluated one synthetic lethal approach for tumors with or without MMR defects.[12] In the case of sporadic tumors evaluated, the majority would be deficient in MMR due to epigenetic repression of an MMR gene (see DNA mismatch repair). The product of gene PD-1 ordinarily represses cytotoxic immune responses. Inhibition of this gene allows a greater immune response. In this Phase II clinical trial with 47 patients, when cancer patients with a defect in MMR in their tumors were exposed to an inhibitor of PD-1, 67% - 78% of patients experienced immune-related progression-free survival. In contrast, for patients without defective MMR, addition of PD-1 inhibitor generated only 11% of patients with immune-related progression-free survival. Thus inhibition of PD-1 is primarily synthetically lethal with MMR defects.
Werner syndrome gene deficiency
[edit]The analysis of 630 human primary tumors in 11 tissues shows that WRN promoter hypermethylation (with loss of expression of WRN protein) is a common event in tumorigenesis.[13] The WRN gene promoter is hypermethylated in about 38% of colorectal cancers and non-small-cell lung carcinomas and in about 20% or so of stomach cancers, prostate cancers, breast cancers, non-Hodgkin lymphomas and chondrosarcomas, plus at significant levels in the other cancers evaluated. The WRN helicase protein is important in homologous recombinational DNA repair and also has roles in non-homologous end joining DNA repair and base excision DNA repair.[14]
Topoisomerase inhibitors are frequently used as chemotherapy for different cancers, though they cause bone marrow suppression, are cardiotoxic and have variable effectiveness.[15] A 2006 retrospective study, with long clinical follow-up, was made of colon cancer patients treated with the topoisomerase inhibitor irinotecan. In this study, 45 patients had hypermethylated WRN gene promoters and 43 patients had unmethylated WRN gene promoters.[13] Irinitecan was more strongly beneficial for patients with hypermethylated WRN promoters (39.4 months survival) than for those with unmethylated WRN promoters (20.7 months survival). Thus, a topoisomerase inhibitor appeared to be synthetically lethal with deficient expression of WRN. Further evaluations have also indicated synthetic lethality of deficient expression of WRN and topoisomerase inhibitors.[16][17][18][19][20]
Clinical and preclinical PARP1 inhibitor synthetic lethality
[edit]As reviewed by Murata et al.,[21] five different PARP1 inhibitors are now undergoing Phase I, II and III clinical trials, to determine if particular PARP1 inhibitors are synthetically lethal in a large variety of cancers, including those in the prostate, pancreas, non-small-cell lung tumors, lymphoma, multiple myeloma, and Ewing sarcoma. In addition, in preclinical studies using cells in culture or within mice, PARP1 inhibitors are being tested for synthetic lethality against epigenetic and mutational deficiencies in about 20 DNA repair defects beyond BRCA1/2 deficiencies. These include deficiencies in PALB2, FANCD2, RAD51, ATM, MRE11, p53, XRCC1 and LSD1.
Preclinical ARID1A synthetic lethality
[edit]ARID1A, a chromatin modifier, is required for non-homologous end joining, a major pathway that repairs double-strand breaks in DNA,[22] and also has transcription regulatory roles.[23] ARID1A mutations are one of the 12 most common carcinogenic mutations.[24] Mutation or epigenetically decreased expression[25] of ARID1A has been found in 17 types of cancer.[26] Pre-clinical studies in cells and in mice show that synthetic lethality for deficient ARID1A expression occurs by either inhibition of the methyltransferase activity of EZH2,[27][28] by inhibition of the DNA repair kinase ATR,[29] or by exposure to the kinase inhibitor dasatinib.[30]
Preclinical RAD52 synthetic lethality
[edit]There are two pathways for homologous recombinational repair of double-strand breaks. The major pathway depends on BRCA1, PALB2 and BRCA2 while an alternative pathway depends on RAD52.[31] Pre-clinical studies, involving epigenetically reduced or mutated BRCA-deficient cells (in culture or injected into mice), show that inhibition of RAD52 is synthetically lethal with BRCA-deficiency.[32]
Side effects
[edit]Although treatments using synthetic lethality can stop or slow progression of cancers and prolong survival, each of the synthetic lethal treatments has some adverse side effects. For example, more than 20% of patients treated with an inhibitor of PD-1 encounter fatigue, rash, pruritus, cough, diarrhea, decreased appetite, constipation or arthralgia.[33] Thus, it is important to determine which DDR deficiency is present, so that only an effective synthetic lethal treatment can be applied, and not unnecessarily subject patients to adverse side effects without a direct benefit.
See also
[edit]References
[edit]- ^ a b Nijman SM (January 2011). "Synthetic lethality: general principles, utility and detection using genetic screens in human cells". FEBS Letters. 585 (1): 1–6. doi:10.1016/j.febslet.2010.11.024. PMC 3018572. PMID 21094158.
- ^ Lord CJ, Ashworth A (March 2017). "PARP inhibitors: Synthetic lethality in the clinic". Science. 355 (6330): 1152–1158. Bibcode:2017Sci...355.1152L. doi:10.1126/science.aam7344. PMC 6175050. PMID 28302823.
- ^ a b Muller FL, Colla S, Aquilanti E, Manzo VE, Genovese G, Lee J, et al. (August 2012). "Passenger deletions generate therapeutic vulnerabilities in cancer". Nature. 488 (7411): 337–42. Bibcode:2012Natur.488..337M. doi:10.1038/nature11331. PMC 3712624. PMID 22895339.
- ^ Ferrari E, Lucca C, Foiani M (November 2010). "A lethal combination for cancer cells: synthetic lethality screenings for drug discovery". European Journal of Cancer. 46 (16): 2889–95. doi:10.1016/j.ejca.2010.07.031. PMID 20724143.
- ^ Hartwell LH, Szankasi P, Roberts CJ, Murray AW, Friend SH (November 1997). "Integrating genetic approaches into the discovery of anticancer drugs". Science. 278 (5340): 1064–8. Bibcode:1997Sci...278.1064H. doi:10.1126/science.278.5340.1064. PMID 9353181.
- ^ Baugh LR, Wen JC, Hill AA, Slonim DK, Brown EL, Hunter CP (2005). "Synthetic lethal analysis of Caenorhabditis elegans posterior embryonic patterning genes identifies conserved genetic interactions". Genome Biology. 6 (5): R45. doi:10.1186/gb-2005-6-5-r45. PMC 1175957. PMID 15892873.
- ^ Hartman JL, Garvik B, Hartwell L (February 2001). "Principles for the buffering of genetic variation". Science. 291 (5506): 1001–4. Bibcode:2001Sci...291.1001H. doi:10.1126/science.291.5506.1001. PMID 11232561.
- ^ Matuo R, Sousa FG, Soares DG, Bonatto D, Saffi J, Escargueil AE, et al. (October 2012). "Saccharomyces cerevisiae as a model system to study the response to anticancer agents". Cancer Chemotherapy and Pharmacology. 70 (4): 491–502. doi:10.1007/s00280-012-1937-4. PMID 22851206. S2CID 8887133.
- ^ Costanzo M, Baryshnikova A, Bellay J, Kim Y, Spear ED, Sevier CS, et al. (January 2010). "The genetic landscape of a cell". Science. 327 (5964): 425–31. Bibcode:2010Sci...327..425C. doi:10.1126/science.1180823. PMC 5600254. PMID 20093466.
- ^ Narayanan L, Fritzell JA, Baker SM, Liskay RM, Glazer PM (April 1997). "Elevated levels of mutation in multiple tissues of mice deficient in the DNA mismatch repair gene Pms2". Proceedings of the National Academy of Sciences of the United States of America. 94 (7): 3122–7. Bibcode:1997PNAS...94.3122N. doi:10.1073/pnas.94.7.3122. PMC 20332. PMID 9096356.
- ^ Hegan DC, Narayanan L, Jirik FR, Edelmann W, Liskay RM, Glazer PM (December 2006). "Differing patterns of genetic instability in mice deficient in the mismatch repair genes Pms2, Mlh1, Msh2, Msh3 and Msh6". Carcinogenesis. 27 (12): 2402–8. doi:10.1093/carcin/bgl079. PMC 2612936. PMID 16728433.
- ^ Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, et al. (June 2015). "PD-1 Blockade in Tumors with Mismatch-Repair Deficiency". The New England Journal of Medicine. 372 (26): 2509–20. doi:10.1056/NEJMoa1500596. PMC 4481136. PMID 26028255.
- ^ a b Agrelo R, Cheng WH, Setien F, Ropero S, Espada J, Fraga MF, et al. (June 2006). "Epigenetic inactivation of the premature aging Werner syndrome gene in human cancer". Proceedings of the National Academy of Sciences of the United States of America. 103 (23): 8822–7. Bibcode:2006PNAS..103.8822A. doi:10.1073/pnas.0600645103. PMC 1466544. PMID 16723399.
- ^ Monnat RJ (October 2010). "Human RECQ helicases: roles in DNA metabolism, mutagenesis and cancer biology". Seminars in Cancer Biology. 20 (5): 329–39. doi:10.1016/j.semcancer.2010.10.002. PMC 3040982. PMID 20934517.
- ^ Pommier Y (January 2013). "Drugging topoisomerases: lessons and challenges". ACS Chemical Biology. 8 (1): 82–95. doi:10.1021/cb300648v. PMC 3549721. PMID 23259582.
- ^ Wang L, Xie L, Wang J, Shen J, Liu B (December 2013). "Correlation between the methylation of SULF2 and WRN promoter and the irinotecan chemosensitivity in gastric cancer". BMC Gastroenterology. 13: 173. doi:10.1186/1471-230X-13-173. PMC 3877991. PMID 24359226.
- ^ Bird JL, Jennert-Burston KC, Bachler MA, Mason PA, Lowe JE, Heo SJ, et al. (February 2012). "Recapitulation of Werner syndrome sensitivity to camptothecin by limited knockdown of the WRN helicase/exonuclease". Biogerontology. 13 (1): 49–62. doi:10.1007/s10522-011-9341-8. PMID 21786128. S2CID 18189226.
- ^ Masuda K, Banno K, Yanokura M, Tsuji K, Kobayashi Y, Kisu I, et al. (October 2012). "Association of epigenetic inactivation of the WRN gene with anticancer drug sensitivity in cervical cancer cells". Oncology Reports. 28 (4): 1146–52. doi:10.3892/or.2012.1912. PMC 3583574. PMID 22797812.
- ^ Futami K, Takagi M, Shimamoto A, Sugimoto M, Furuichi Y (October 2007). "Increased chemotherapeutic activity of camptothecin in cancer cells by siRNA-induced silencing of WRN helicase". Biological & Pharmaceutical Bulletin. 30 (10): 1958–61. doi:10.1248/bpb.30.1958. PMID 17917271.
- ^ Futami K, Ishikawa Y, Goto M, Furuichi Y, Sugimoto M (May 2008). "Role of Werner syndrome gene product helicase in carcinogenesis and in resistance to genotoxins by cancer cells". Cancer Science. 99 (5): 843–8. doi:10.1111/j.1349-7006.2008.00778.x. PMC 11158842. PMID 18312465. S2CID 21078795.
- ^ Murata S, Zhang C, Finch N, Zhang K, Campo L, Breuer EK (2016). "Predictors and Modulators of Synthetic Lethality: An Update on PARP Inhibitors and Personalized Medicine". BioMed Research International. 2016: 2346585. doi:10.1155/2016/2346585. PMC 5013223. PMID 27642590.
- ^ Watanabe R, Ui A, Kanno S, Ogiwara H, Nagase T, Kohno T, Yasui A (May 2014). "SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability". Cancer Research. 74 (9): 2465–75. doi:10.1158/0008-5472.CAN-13-3608. PMID 24788099.
- ^ Raab JR, Resnick S, Magnuson T (December 2015). "Genome-Wide Transcriptional Regulation Mediated by Biochemically Distinct SWI/SNF Complexes". PLOS Genetics. 11 (12): e1005748. doi:10.1371/journal.pgen.1005748. PMC 4699898. PMID 26716708.
- ^ Lawrence MS, Stojanov P, Mermel CH, Robinson JT, Garraway LA, Golub TR, et al. (January 2014). "Discovery and saturation analysis of cancer genes across 21 tumour types". Nature. 505 (7484): 495–501. Bibcode:2014Natur.505..495L. doi:10.1038/nature12912. PMC 4048962. PMID 24390350.
- ^ Zhang X, Sun Q, Shan M, Niu M, Liu T, Xia B, et al. (2013). "Promoter hypermethylation of ARID1A gene is responsible for its low mRNA expression in many invasive breast cancers". PLOS ONE. 8 (1): e53931. Bibcode:2013PLoSO...853931Z. doi:10.1371/journal.pone.0053931. PMC 3549982. PMID 23349767.
- ^ Wu JN, Roberts CW (January 2013). "ARID1A mutations in cancer: another epigenetic tumor suppressor?". Cancer Discovery. 3 (1): 35–43. doi:10.1158/2159-8290.CD-12-0361. PMC 3546152. PMID 23208470.
- ^ Bitler BG, Aird KM, Garipov A, Li H, Amatangelo M, Kossenkov AV, et al. (March 2015). "Synthetic lethality by targeting EZH2 methyltransferase activity in ARID1A-mutated cancers". Nature Medicine. 21 (3): 231–8. doi:10.1038/nm.3799. PMC 4352133. PMID 25686104.
- ^ Kim KH, Kim W, Howard TP, Vazquez F, Tsherniak A, Wu JN, et al. (December 2015). "SWI/SNF-mutant cancers depend on catalytic and non-catalytic activity of EZH2". Nature Medicine. 21 (12): 1491–6. doi:10.1038/nm.3968. PMC 4886303. PMID 26552009.
- ^ Williamson CT, Miller R, Pemberton HN, Jones SE, Campbell J, Konde A, et al. (December 2016). "ATR inhibitors as a synthetic lethal therapy for tumours deficient in ARID1A". Nature Communications. 7: 13837. Bibcode:2016NatCo...713837W. doi:10.1038/ncomms13837. PMC 5159945. PMID 27958275.
- ^ Miller RE, Brough R, Bajrami I, Williamson CT, McDade S, Campbell J, et al. (July 2016). "Synthetic Lethal Targeting of ARID1A-Mutant Ovarian Clear Cell Tumors with Dasatinib". Molecular Cancer Therapeutics. 15 (7): 1472–84. doi:10.1158/1535-7163.MCT-15-0554. PMID 27364904.
- ^ Lok BH, Carley AC, Tchang B, Powell SN (July 2013). "RAD52 inactivation is synthetically lethal with deficiencies in BRCA1 and PALB2 in addition to BRCA2 through RAD51-mediated homologous recombination". Oncogene. 32 (30): 3552–8. doi:10.1038/onc.2012.391. PMC 5730454. PMID 22964643.
- ^ Cramer-Morales K, Nieborowska-Skorska M, Scheibner K, Padget M, Irvine DA, Sliwinski T, et al. (August 2013). "Personalized synthetic lethality induced by targeting RAD52 in leukemias identified by gene mutation and expression profile". Blood. 122 (7): 1293–304. doi:10.1182/blood-2013-05-501072. PMC 3744994. PMID 23836560.
- ^ Villadolid J, Amin A (October 2015). "Immune checkpoint inhibitors in clinical practice: update on management of immune-related toxicities". Translational Lung Cancer Research. 4 (5): 560–75. doi:10.3978/j.issn.2218-6751.2015.06.06. PMC 4630514. PMID 26629425.
External links
[edit]- Data Repository of Yeast Genetic INteractions
- Saccharomyces Genome Deletion Project
- SynLethDB Database
