Monoamine neurotoxin
A monoamine neurotoxin, or monoaminergic neurotoxin, is a drug that selectively damages or destroys monoaminergic neurons.[1] Monoaminergic neurons are neurons that signal via stimulation by monoamine neurotransmitters including serotonin, dopamine, and norepinephrine.[1]
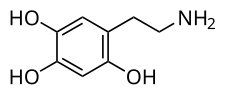
Examples of monoamine neurotoxins include the serotonergic neurotoxins para-chloroamphetamine (PCA), methylenedioxymethamphetamine (MDMA), and 5,7-dihydroxytryptamine (5,7-DHT);[2] the dopaminergic neurotoxins oxidopamine (6-hydroxydopamine), MPTP, and methamphetamine; and the noradrenergic neurotoxins oxidopamine and DSP-4.[1]
In the case of serotonergic neurotoxins like MDMA, research suggests that simultaneous induction of serotonin and dopamine release, serotonin depletion, dopamine uptake and metabolism, hyperthermia, oxidative stress and antioxidant depletion, and/or drug metabolites may all be involved in the neurotoxicity.[3][4] On the other hand, there is evidence that drug metabolites may not be involved.[3][4]
Dopaminergic neurotoxins can induce a Parkinson's disease-like condition in animals and humans.[1][5] Serotonergic neurotoxins have been associated with cognitive and memory deficits and psychiatric changes.[6][7][8][9]
List of monoamine neurotoxins
[edit]Serotonergic neurotoxins
[edit]Phenethylamines
[edit]- 2,4-Dichloroamphetamine (2,4-DCA)[10]
- 2,4,5-Trihydroxyamphetamine (2,4,5-THA)[11]
- 2,4,5-Trihydroxymethamphetamine (2,4,5-THMA)[11]
- 3-Chloroamphetamine (3-CA)[10][12]
- 3,4-Dichloroamphetamine (3,4-DCA)[10]
- 3,4-Dihydroxyamphetamine (HHA; 3,4-DHA; α-methyldopamine; α-Me-DA)[2]
- 3,4-Dihydroxymethamphetamine (HHMA; 3,4-DHMA; α-methylepinine; α,N-dimethyldopamine)[2]
- 3,4-Methylenedioxyamphetamine (MDA)[1][13][2][11]
- 3,4-Methylenedioxyethylamphetamine (MDEA)[13][14]
- 3,4-Methylenedioxymethamphetamine (MDMA)[1][2][15][16]
- 4-Chlorophenylisobutylamine (4-CAB; 4-chloro-α-desmethyl-α-ethylamphetamine; α-ethyl-PCA)[13]
- 5-MAPB[17]
- Fenfluramine[1][18][19][20]
- Mephedrone[21]
- Methamphetamine[1][16][11]
- Methylbenzodioxolylbutanamine (MBDB)[13][14]
- Methylone[21]
- Norfenfluramine[20][22]
- para-Bromoamphetamine (PBA; 4-bromoamphetamine; 4-BA)[23]
- para-Chloroamphetamine (PCA; 4-chloroamphetamine; 4-CA)[1][2][14]
- para-Chloromethamphetamine (PCMA; 4-chloromethamphetamine; 4-PCMA)[10][24]
- para-Iodoamphetamine (PIA; 4-iodoamphetamine; 4-IA)[13][25]
Tryptamines
[edit]- 4,5-Dihydroxytryptamine (4,5-DHT)[26][27]
- 5,6-Dihydroxytryptamine (5,6-DHT)[28][1][2]
- 5,7-Dihydroxytryptamine (5,7-DHT)[28][1][2]
- 6,7-Dihydroxytryptamine (6,7-DHT)[26][29]
- α-Ethyltryptamine (αET)[14][30][31]
2-Aminoindans
[edit]- 5-Iodo-2-aminoindan (5-IAI) (weak)[32][14][13]
- 5-Methoxy-6-methyl-2-aminoindane (MMAI) (weak; alone and with amphetamine)[33][34][35]
- 5,6-Methylenedioxy-2-aminoindan (MDAI) (weak; alone and with amphetamine)[36][13][37]
MPTP-related
[edit]Dopaminergic neurotoxins
[edit]Phenethylamines
[edit]- 2,4,5-Trihydroxyamphetamine (2,4,5-THA)[11]
- 2,4,5-Trihydroxymethamphetamine (2,4,5-THMA)[11]
- 3,4-Methylenedioxymethamphetamine (MDMA) (in mice but not in humans)[16][8]
- 6-Hydroxydopa (6-OH-DOPA, 6-OHDOPA)[1][40][41]
- 6-Hydroxydopamine quinone (6-OHDA quinone; oxidopamine quinone)[42][43]
- Amphetamine[1]
- Mephedrone[21]
- Methamphetamine[1][15][16]
- Methylone[21]
- Oxidopamine (6-hydroxydopamine; 6-OHDA)[44][45][42]
Dopamine and metabolites
[edit]- 3,4-Dihydroxyphenylacetaldehyde (DOPAL; dopamine aldehyde)[46][47]
- 5-S-Cysteinyldopamine (5-S-CyS-DA)[48]
- DOPA quinone[49][50]
- DOPAL quinone[51]
- Dopamine[52]
- Dopamine quinone[49][50]
- N-Methylnorsalsolinol[53]
- Norsalsolinol[53]
- Salsolinol[53][54]
Tryptamines
[edit]- 5,6-Dihydroxytryptamine (5,6-DHT)[28][55]
- 6,7-Dihydroxytryptamine (6,7-DHT)[26][29]
MPTP-related
[edit]- 2′-CH3-MPTP (2′-methyl-MPTP)[56][57][58][59][60]
- Haloperidol[1][38]
- HPP+ (haloperidol pyridinium)[1][38]
- HPTP[1][39]
- MPP+ (cyperquat)[61][62]
- MPTP[61]
Pesticides
[edit]- Benomyl[63]
- Daidzin[63]
- Dieldrin[63]
- Fenpropathrin[64][65][66]
- Mancozeb[67]
- Maneb[67]
- Paraquat[64][67][68]
- Rotenone[1][64][67][69]
- Ziram[63]
Others
[edit]Noradrenergic neurotoxins
[edit]Phenethylamines and related
[edit]- 2,4,5-Trihydroxyamphetamine (2,4,5-THA)[11]
- 3,4-Methylenedioxyamphetamine (MDA)[11]
- 3,4-Dihydroxyphenylglycolaldehyde (DOPEGAL; norepinephrine/epinephrine aldehyde)[73]
- 6-Hydroxydopa (6-OH-DOPA, 6-OHDOPA)[1][40][41]
- DSP-4[74][75]
- Oxidopamine (6-hydroxydopamine; 6-OHDA)[44][42]
- Xylamine[1]
Tryptamines and related
[edit]- 4,5-Dihydroxytryptamine (4,5-DHT)[26][27]
- 5,6-Dihydroxytryptamine (5,6-DHT)[28][55]
- 5,7-Dihydroxytryptamine (5,7-DHT)[28][55]
MPTP-related
[edit]- 2′-NH2-MPTP (2′-amino-MPTP)[1]
Unsorted or unknown
[edit]See also
[edit]References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y Kostrzewa RM (2022). "Survey of Selective Monoaminergic Neurotoxins Targeting Dopaminergic, Noradrenergic, and Serotoninergic Neurons". Handbook of Neurotoxicity. Cham: Springer International Publishing. pp. 159–198. doi:10.1007/978-3-031-15080-7_53. ISBN 978-3-031-15079-1.
- ^ a b c d e f g h Baumgarten HG, Lachenmayer L (2004). "Serotonin neurotoxins--past and present". Neurotox Res. 6 (7–8): 589–614. doi:10.1007/BF03033455. PMID 15639791.
- ^ a b Baggott M, Mendelson J (2001). "Does MDMA Cause Brain Damage?". In Holland J (ed.). Ecstasy: The Complete Guide: A Comprehensive Look at the Risks and Benefits of MDMA. Inner Traditions/Bear. pp. 110–145, 396–404. ISBN 978-0-89281-857-0. Retrieved 24 November 2024.
While a single injection of MDMA into the brain (intracerebroventricularly) had no effect on TPH activity, slow infusion of 1 mg/kg MDMA into the brain over 1 hr produced enough oxidative stress to acutely reduce TPH activity (Schmidt and Taylor 1988). The acute decrease in TPH activity is an early effect of MDMA and can be measured at post 15 min (Stone et al. 1989b). TPH inactivation can also be produced by non-neurotoxic MDMA doses (Schmidt and Taylor 1988; Stone et al. 1989a; Stone et al. 1989b). It therefore appears that MDMA rapidly induces oxidative stress but only produces neurotoxicity when endogenous free radical scavenging systems are overwhelmed.
- ^ a b Sprague JE, Everman SL, Nichols DE (June 1998). "An integrated hypothesis for the serotonergic axonal loss induced by 3,4-methylenedioxymethamphetamine". Neurotoxicology. 19 (3): 427–441. PMID 9621349.
- ^ Grünblatt E, Mandel S, Youdim MB (April 2000). "MPTP and 6-hydroxydopamine-induced neurodegeneration as models for Parkinson's disease: neuroprotective strategies". J Neurol. 247 (Suppl 2): II95–102. doi:10.1007/pl00022909. PMID 10991672.
- ^ Parrott AC (April 2002). "Recreational Ecstasy/MDMA, the serotonin syndrome, and serotonergic neurotoxicity". Pharmacol Biochem Behav. 71 (4): 837–844. doi:10.1016/s0091-3057(01)00711-0. PMID 11888574.
- ^ Parrott AC (September 2013). "MDMA, serotonergic neurotoxicity, and the diverse functional deficits of recreational 'Ecstasy' users". Neurosci Biobehav Rev. 37 (8): 1466–1484. doi:10.1016/j.neubiorev.2013.04.016. PMID 23660456.
- ^ a b Aguilar MA, García-Pardo MP, Parrott AC (January 2020). "Of mice and men on MDMA: A translational comparison of the neuropsychobiological effects of 3,4-methylenedioxymethamphetamine ('Ecstasy')". Brain Res. 1727: 146556. doi:10.1016/j.brainres.2019.146556. PMID 31734398.
- ^ Montgomery C, Roberts CA (January 2022). "Neurological and cognitive alterations induced by MDMA in humans" (PDF). Exp Neurol. 347: 113888. doi:10.1016/j.expneurol.2021.113888. PMID 34624331.
- ^ a b c d Biel JH, Bopp BA (1978). "Amphetamines: Structure-Activity Relationships". Stimulants. Boston, MA: Springer US. pp. 1–39. doi:10.1007/978-1-4757-0510-2_1. ISBN 978-1-4757-0512-6.
- ^ a b c d e f g h Gibb JW, Johnson M, Elayan I, Lim HK, Matsuda L, Hanson GR (1997). "Neurotoxicity of amphetamines and their metabolites" (PDF). NIDA Res Monogr. 173: 128–145. PMID 9260187.
- ^ Fuller RW, Baker JC (November 1974). "Long-lasting reduction of brain 5-hydroxytryptamine concentration by 3-chloramphetamine and 4-chloroamphetamine in iprindole-treated rats". J Pharm Pharmacol. 26 (11): 912–914. doi:10.1111/j.2042-7158.1974.tb09206.x. PMID 4156568.
- ^ a b c d e f g Nichols DE, Marona-Lewicka D, Huang X, Johnson MP (1993). "Novel serotonergic agents". Drug des Discov. 9 (3–4): 299–312. PMID 8400010.
- ^ a b c d e Oeri HE (May 2021). "Beyond ecstasy: Alternative entactogens to 3,4-methylenedioxymethamphetamine with potential applications in psychotherapy". J Psychopharmacol. 35 (5): 512–536. doi:10.1177/0269881120920420. PMC 8155739. PMID 32909493.
- ^ a b Seiden LS, Sabol KE (1996). "Methamphetamine and methylenedioxymethamphetamine neurotoxicity: possible mechanisms of cell destruction" (PDF). NIDA Res Monogr. 163: 251–276. PMID 8809863.
- ^ a b c d Itzhak Y, Achat-Mendes C (May 2004). "Methamphetamine and MDMA (ecstasy) neurotoxicity: 'of mice and men'". IUBMB Life. 56 (5): 249–255. doi:10.1080/15216540410001727699. PMID 15370888.
- ^ Johnson CB, Burroughs RL, Baggott MJ, Davidson CJ, Perrine SA, Baker LE (2022). 314.03 / RR6 - Locomotor stimulant effects and persistent serotonin depletions following [1-Benzofuran-5-yl)-N-methylpropan-2-amine (5-MAPB) treatment in Sprague-Dawley rats. Society for Neuroscience Conference, Nov. 14, 2022, San Diego, CA.
5-MAPB has been marketed as a less neurotoxic analogue of MDMA, but no studies have addressed whether 5-MAPB can cause the long lasting serotonergic changes seen with high or repeated MDMA dosing. [...] Neurochemical analyses indicated a statistically significant reduction in 5‑HT and 5-HIAA in all brain regions assessed 24 hours and two weeks after 6 mg/kg 5‑MAPB, with no statistically significant differences in monoamine levels between 1.2 mg/kg and saline-treated rats. There were also non-significant trends for reductions in striatal dopamine at both time intervals after 6 mg/kg 5-MAPB. These results show that 5-MAPB can dose-dependently produce persistent changes in 5-HT and 5-HIAA that appear analogous to those produced by MDMA.
- ^ McCann UD, Seiden LS, Rubin LJ, Ricaurte GA (August 1997). "Brain serotonin neurotoxicity and primary pulmonary hypertension from fenfluramine and dexfenfluramine. A systematic review of the evidence". JAMA. 278 (8): 666–672. doi:10.1001/jama.1997.03550080076043. PMID 9272900.
- ^ Rothman RB, Baumann MH (April 2002). "Serotonin releasing agents. Neurochemical, therapeutic and adverse effects". Pharmacol Biochem Behav. 71 (4): 825–836. doi:10.1016/s0091-3057(01)00669-4. PMID 11888573.
- ^ a b Johnson MP, Nichols DE (May 1990). "Comparative serotonin neurotoxicity of the stereoisomers of fenfluramine and norfenfluramine". Pharmacol Biochem Behav. 36 (1): 105–109. doi:10.1016/0091-3057(90)90133-3. PMID 2140899.
- ^ a b c d Daziani G, Lo Faro AF, Montana V, Goteri G, Pesaresi M, Bambagiotti G, et al. (March 2023). "Synthetic Cathinones and Neurotoxicity Risks: A Systematic Review". Int J Mol Sci. 24 (7): 6230. doi:10.3390/ijms24076230. PMC 10093970. PMID 37047201.
- ^ Caccia S, Anelli M, Ferrarese A, Fracasso C, Garattini S (March 1993). "The role of d-norfenfluramine in the indole-depleting effect of d-fenfluramine in the rat". Eur J Pharmacol. 233 (1): 71–77. doi:10.1016/0014-2999(93)90350-q. PMID 7682511.
- ^ Harvey JA (June 1978). "Neurotoxic action of halogenated amphetamines". Ann N Y Acad Sci. 305 (1): 289–304. Bibcode:1978NYASA.305..289H. doi:10.1111/j.1749-6632.1978.tb31530.x. PMID 81648.
- ^ Shulgin AT (1978). "Psychotomimetic Drugs: Structure-Activity Relationships". Stimulants. Boston, MA: Springer US. pp. 243–333. doi:10.1007/978-1-4757-0510-2_6. ISBN 978-1-4757-0512-6.
- ^ Iversen L, White M, Treble R (December 2014). "Designer psychostimulants: pharmacology and differences". Neuropharmacology. 87: 59–65. doi:10.1016/j.neuropharm.2014.01.015. PMID 24456744.
- ^ a b c d Nobin A, Björklund A (June 1978). "Degenerative effects of various neurotoxic indoleamines on central monoamine neurons". Ann N Y Acad Sci. 305: 305–327. doi:10.1111/j.1749-6632.1978.tb31531.x. PMID 360938.
- ^ a b Björklund A, Nobin A, Stenevi U (December 1973). "The use of neurotoxic dihydroxytryptamines as tools for morphological studies and localized lesioning of central indolamine neurons". Z Zellforsch Mikrosk Anat. 145 (4): 479–501. doi:10.1007/BF00306720. PMID 4774982.
- ^ a b c d e Paterak J, Stefański R (2022). "5,6- and 5,7-Dihydroxytryptamines as Serotoninergic Neurotoxins". Handbook of Neurotoxicity. Cham: Springer International Publishing. pp. 691–717. doi:10.1007/978-3-031-15080-7_76. ISBN 978-3-031-15079-1.
- ^ a b Massotti M, Scotti de Carolis A, Longo VG (1974). "Effects of three dihydroxylated derivatives of tryptamine on the behavior and on brain amine content in mice". Pharmacol Biochem Behav. 2 (6): 769–776. doi:10.1016/0091-3057(74)90109-9. PMID 4549398.
- ^ Glennon RA, Dukat MG (December 2023). "α-Ethyltryptamine: A Ratiocinatory Review of a Forgotten Antidepressant". ACS Pharmacol Transl Sci. 6 (12): 1780–1789. doi:10.1021/acsptsci.3c00139. PMC 10714429. PMID 38093842.
- ^ Huang XM, Johnson MP, Nichols DE (July 1991). "Reduction in brain serotonin markers by alpha-ethyltryptamine (Monase)". Eur J Pharmacol. 200 (1): 187–190. doi:10.1016/0014-2999(91)90686-k. PMID 1722753.
- ^ Sainsbury PD, Kicman AT, Archer RP, King LA, Braithwaite RA (2011). "Aminoindanes--the next wave of 'legal highs'?". Drug Test Anal. 3 (7–8): 479–482. doi:10.1002/dta.318. PMID 21748859.
- ^ Brandt SD, Braithwaite RA, Evans-Brown M, Kicman AT (2013). "Aminoindane Analogues". Novel Psychoactive Substances. Elsevier. pp. 261–283. doi:10.1016/b978-0-12-415816-0.00011-0. ISBN 978-0-12-415816-0.
- ^ Johnson MP, Nichols DE (July 1991). "Combined administration of a non-neurotoxic 3,4-methylenedioxymethamphetamine analogue with amphetamine produces serotonin neurotoxicity in rats". Neuropharmacology. 30 (7): 819–822. doi:10.1016/0028-3908(91)90192-e. PMID 1717873.
- ^ Johnson MP, Conarty PF, Nichols DE (July 1991). "[3H]monoamine releasing and uptake inhibition properties of 3,4-methylenedioxymethamphetamine and p-chloroamphetamine analogues". Eur J Pharmacol. 200 (1): 9–16. doi:10.1016/0014-2999(91)90659-e. PMID 1685125.
- ^ Corkery JM, Elliott S, Schifano F, Corazza O, Ghodse AH (July 2013). "MDAI (5,6-methylenedioxy-2-aminoindane; 6,7-dihydro-5H-cyclopenta[f][1,3]benzodioxol-6-amine; 'sparkle'; 'mindy') toxicity: a brief overview and update". Hum Psychopharmacol. 28 (4): 345–355. doi:10.1002/hup.2298. PMID 23881883.
- ^ Johnson MP, Huang XM, Nichols DE (December 1991). "Serotonin neurotoxicity in rats after combined treatment with a dopaminergic agent followed by a nonneurotoxic 3,4-methylenedioxymethamphetamine (MDMA) analogue". Pharmacol Biochem Behav. 40 (4): 915–922. doi:10.1016/0091-3057(91)90106-c. PMID 1726189.
- ^ a b c d Igarashi K (1998). "The Possible Role of an Active Metafbollte Derived from the Neuroleptic Agent Haloperidol in Drug-Induced Parkinsonism". Journal of Toxicology: Toxin Reviews. 17 (1): 27–38. doi:10.3109/15569549809006488. ISSN 0731-3837.
- ^ a b c Castagnoli N, Castagnoli KP, Van der Schyf CJ, Usuki E, Igarashi K, Steyn SJ, et al. (1999). "Enzyme-catalyzed bioactivation of cyclic tertiary amines to form potential neurotoxins". Pol J Pharmacol. 51 (1): 31–38. PMID 10389142.
- ^ a b Kostrzewa RM (2016). "Perinatal Lesioning and Lifelong Effects of the Noradrenergic Neurotoxin 6-Hydroxydopa". Curr Top Behav Neurosci. Current Topics in Behavioral Neurosciences. 29: 43–50. doi:10.1007/7854_2015_414. ISBN 978-3-319-34134-7. PMID 26660536.
- ^ a b Kostrzewa RM, Brus R (1998). "Destruction of catecholamine-containing neurons by 6-hydroxydopa, an endogenous amine oxidase cofactor". Amino Acids. 14 (1–3): 175–179. doi:10.1007/BF01345259. PMID 9871458.
- ^ a b c Varešlija D, Tipton KF, Davey GP, McDonald AG (February 2020). "6-Hydroxydopamine: a far from simple neurotoxin". J Neural Transm (Vienna). 127 (2): 213–230. doi:10.1007/s00702-019-02133-6. PMID 31894418.
- ^ Villa M, Muñoz P, Ahumada-Castro U, Paris I, Jiménez A, Martínez I, et al. (July 2013). "One-electron reduction of 6-hydroxydopamine quinone is essential in 6-hydroxydopamine neurotoxicity". Neurotox Res. 24 (1): 94–101. doi:10.1007/s12640-013-9382-7. PMID 23385626.
- ^ a b Glinka Y, Gassen M, Youdim MB (1997). "Mechanism of 6-hydroxydopamine neurotoxicity". Advances in Research on Neurodegeneration. Journal of Neural Transmission. Supplementa. Vol. 50. pp. 55–66. doi:10.1007/978-3-7091-6842-4_7. ISBN 978-3-211-82898-4. PMID 9120425.
{{cite book}}:|journal=ignored (help) - ^ Hernandez-Baltazar D, Zavala-Flores LM, Villanueva-Olivo A (October 2017). "The 6-hydroxydopamine model and parkinsonian pathophysiology: Novel findings in an older model" (PDF). Neurologia. 32 (8): 533–539. doi:10.1016/j.nrl.2015.06.011. PMID 26304655.
- ^ Goldstein DS (February 2020). "The catecholaldehyde hypothesis: where MAO fits in". J Neural Transm (Vienna). 127 (2): 169–177. doi:10.1007/s00702-019-02106-9. PMC 10680281. PMID 31807952.
- ^ Goldstein DS (June 2021). "The Catecholaldehyde Hypothesis for the Pathogenesis of Catecholaminergic Neurodegeneration: What We Know and What We Do Not Know". Int J Mol Sci. 22 (11): 5999. doi:10.3390/ijms22115999. PMC 8199574. PMID 34206133.
- ^ Badillo-Ramírez I, Saniger JM, Rivas-Arancibia S (October 2019). "5-S-cysteinyl-dopamine, a neurotoxic endogenous metabolite of dopamine: Implications for Parkinson's disease". Neurochem Int. 129: 104514. doi:10.1016/j.neuint.2019.104514. PMID 31369776.
- ^ a b Miyazaki I, Asanuma M (April 2009). "Approaches to prevent dopamine quinone-induced neurotoxicity". Neurochem Res. 34 (4): 698–706. doi:10.1007/s11064-008-9843-1. PMID 18770028.
- ^ a b Asanuma M, Miyazaki I, Ogawa N (2003). "Dopamine- or L-DOPA-induced neurotoxicity: the role of dopamine quinone formation and tyrosinase in a model of Parkinson's disease". Neurotox Res. 5 (3): 165–176. doi:10.1007/BF03033137. PMID 12835121.
- ^ Goldstein DS, Sharabi Y (January 2019). "The heart of PD: Lewy body diseases as neurocardiologic disorders". Brain Res. 1702: 74–84. doi:10.1016/j.brainres.2017.09.033. PMC 10712237. PMID 29030055.
- ^ Chakrabarti S, Bisaglia M (April 2023). "Oxidative Stress and Neuroinflammation in Parkinson's Disease: The Role of Dopamine Oxidation Products". Antioxidants. 12 (4): 955. doi:10.3390/antiox12040955. PMC 10135711. PMID 37107329.
- ^ a b c Cao Y, Li B, Ismail N, Smith K, Li T, Dai R, et al. (November 2021). "Neurotoxicity and Underlying Mechanisms of Endogenous Neurotoxins". Int J Mol Sci. 22 (23): 12805. doi:10.3390/ijms222312805. PMC 8657695. PMID 34884606.
- ^ Kurnik-Łucka M, Panula P, Bugajski A, Gil K (February 2018). "Salsolinol: an Unintelligible and Double-Faced Molecule-Lessons Learned from In Vivo and In Vitro Experiments". Neurotox Res. 33 (2): 485–514. doi:10.1007/s12640-017-9818-6. PMC 5766726. PMID 29063289.
- ^ a b c Baumgarten HG, Klemm HP, Lachenmayer L, Björklund A, Lovenberg W, Schlossberger HG (June 1978). "Mode and mechanism of action of neurotoxic indoleamines: a review and a progress report". Ann N Y Acad Sci. 305 (1): 3–24. Bibcode:1978NYASA.305....3B. doi:10.1111/j.1749-6632.1978.tb31507.x. PMID 360937.
- ^ Maret G, Testa B, Jenner P, el Tayar N, Carrupt PA (1990). "The MPTP story: MAO activates tetrahydropyridine derivatives to toxins causing parkinsonism". Drug Metab Rev. 22 (4): 291–332. doi:10.3109/03602539009041087. PMID 2253555.
- ^ Manaye KF, Sonsalla PK, Barnett G, Heikkila RE, Woodward DJ, Smith WK, et al. (July 1989). "1-Methyl-4-(2'-methylphenyl)-1,2,3,6-tetrahydropyridine (2'CH3-MPTP)-induced degeneration of mesostriatal dopaminergic neurons in the mouse: biochemical and neuroanatomical studies". Brain Res. 491 (2): 307–315. doi:10.1016/0006-8993(89)90065-6. PMID 2765888.
- ^ Heikkila RE, Sieber BA, Manzino L, Sonsalla PK (June 1989). "Some features of the nigrostriatal dopaminergic neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in the mouse". Mol Chem Neuropathol. 10 (3): 171–183. doi:10.1007/BF03159727. PMID 2669769.
- ^ Youngster SK, Duvoisin RC, Hess A, Sonsalla PK, Kindt MV, Heikkila RE (March 1986). "1-Methyl-4-(2'-methylphenyl)-1,2,3,6-tetrahydropyridine (2'-CH3-MPTP) is a more potent dopaminergic neurotoxin than MPTP in mice". Eur J Pharmacol. 122 (2): 283–287. doi:10.1016/0014-2999(86)90115-9. PMID 3486770.
- ^ Rose S, Nomoto M, Jackson EA, Gibb WR, Jenner P, Marsden CD (May 1990). "1-Methyl-4-(2'-methylphenyl)-1,2,3,6-tetrahydropyridine (2'-methyl-MPTP) is less neurotoxic than MPTP in the common marmoset". Eur J Pharmacol. 181 (1–2): 97–103. doi:10.1016/0014-2999(90)90249-6. PMID 2117541.
- ^ a b Przedborski S, Vila M (2001). "MPTP: a review of its mechanisms of neurotoxicity". Clinical Neuroscience Research. 1 (6): 407–418. doi:10.1016/S1566-2772(01)00019-6.
- ^ Dinis-Oliveira RJ, Remião F, Carmo H, Duarte JA, Navarro AS, Bastos ML, et al. (December 2006). "Paraquat exposure as an etiological factor of Parkinson's disease". Neurotoxicology. 27 (6): 1110–1122. Bibcode:2006NeuTx..27.1110D. doi:10.1016/j.neuro.2006.05.012. PMID 16815551.
Ironically, in the 1960s, MPP+ itself had been tested as an herbicide under the commercial name of cyperquat (Di Monte, 2001).
- ^ a b c d e Masato A, Plotegher N, Boassa D, Bubacco L (August 2019). "Impaired dopamine metabolism in Parkinson's disease pathogenesis". Mol Neurodegener. 14 (1): 35. doi:10.1186/s13024-019-0332-6. PMC 6728988. PMID 31488222.
- ^ a b c Arsuffi-Marcon R, Souza LG, Santos-Miranda A, Joviano-Santos JV (March 2024). "Neurotoxicity of Pyrethroids in neurodegenerative diseases: From animals' models to humans' studies". Chem Biol Interact. 391: 110911. Bibcode:2024CBI...39110911A. doi:10.1016/j.cbi.2024.110911. PMID 38367681.
- ^ Xiong J, Zhang X, Huang J, Chen C, Chen Z, Liu L, et al. (March 2016). "Fenpropathrin, a Widely Used Pesticide, Causes Dopaminergic Degeneration". Mol Neurobiol. 53 (2): 995–1008. doi:10.1007/s12035-014-9057-2. PMC 5333774. PMID 25575680.
- ^ Jiao Z, Wu Y, Qu S (2020). "Fenpropathrin induces degeneration of dopaminergic neurons via disruption of the mitochondrial quality control system". Cell Death Discov. 6: 78. doi:10.1038/s41420-020-00313-y. PMC 7447795. PMID 32884840.
- ^ a b c d Bastías-Candia S, Zolezzi JM, Inestrosa NC (February 2019). "Revisiting the Paraquat-Induced Sporadic Parkinson's Disease-Like Model". Mol Neurobiol. 56 (2): 1044–1055. doi:10.1007/s12035-018-1148-z. PMID 29862459.
- ^ Kuter K, Smiałowska M, Wierońska J, Zieba B, Wardas J, Pietraszek M, et al. (June 2007). "Toxic influence of subchronic paraquat administration on dopaminergic neurons in rats". Brain Res. 1155: 196–207. doi:10.1016/j.brainres.2007.04.018. PMID 17493592.
- ^ Goldstein DS, Sullivan P, Cooney A, Jinsmaa Y, Kopin IJ, Sharabi Y (April 2015). "Rotenone decreases intracellular aldehyde dehydrogenase activity: implications for the pathogenesis of Parkinson's disease". J Neurochem. 133 (1): 14–25. doi:10.1111/jnc.13042. PMC 4361358. PMID 25645689.
- ^ Doorn JA, Florang VR, Schamp JH, Vanle BC (January 2014). "Aldehyde dehydrogenase inhibition generates a reactive dopamine metabolite autotoxic to dopamine neurons". Parkinsonism Relat Disord. 20 Suppl 1 (1): S73–S75. doi:10.1016/S1353-8020(13)70019-1. PMC 3932615. PMID 24262193.
- ^ Legros H, Dingeval MG, Janin F, Costentin J, Bonnet JJ (March 2004). "Toxicity of a treatment associating dopamine and disulfiram for catecholaminergic neuroblastoma SH-SY5Y cells: relationships with 3,4-dihydroxyphenylacetaldehyde formation". Neurotoxicology. 25 (3): 365–375. Bibcode:2004NeuTx..25..365L. doi:10.1016/S0161-813X(03)00148-7. PMID 15019299.
- ^ Tiernan CT, Edwin EA, Hawong HY, Ríos-Cabanillas M, Goudreau JL, Atchison WD, et al. (April 2015). "Methylmercury impairs canonical dopamine metabolism in rat undifferentiated pheochromocytoma (PC12) cells by indirect inhibition of aldehyde dehydrogenase". Toxicol Sci. 144 (2): 347–356. doi:10.1093/toxsci/kfv001. PMC 4372664. PMID 25601988.
- ^ Marchitti SA, Deitrich RA, Vasiliou V (June 2007). "Neurotoxicity and metabolism of the catecholamine-derived 3,4-dihydroxyphenylacetaldehyde and 3,4-dihydroxyphenylglycolaldehyde: the role of aldehyde dehydrogenase". Pharmacol Rev. 59 (2): 125–150. doi:10.1124/pr.59.2.1. PMID 17379813.
- ^ Ross SB, Stenfors C (January 2015). "DSP4, a selective neurotoxin for the locus coeruleus noradrenergic system. A review of its mode of action". Neurotox Res. 27 (1): 15–30. doi:10.1007/s12640-014-9482-z. PMID 24964753.
- ^ Jaim-Etcheverry G, Zieher LM (April 1980). "DSP-4: a novel compound with neurotoxic effects on noradrenergic neurons of adult and developing rats". Brain Res. 188 (2): 513–523. doi:10.1016/0006-8993(80)90049-9. PMID 7370771.
- ^ Cagle BS, Crawford RA, Doorn JA (February 2019). "Biogenic Aldehyde-Mediated Mechanisms of Toxicity in Neurodegenerative Disease". Curr Opin Toxicol. 13: 16–21. Bibcode:2019COTox..13...16C. doi:10.1016/j.cotox.2018.12.002. PMC 6625780. PMID 31304429.
- ^ Matveychuk D, MacKenzie EM, Kumpula D, Song MS, Holt A, Kar S, et al. (January 2022). "Overview of the Neuroprotective Effects of the MAO-Inhibiting Antidepressant Phenelzine". Cell Mol Neurobiol. 42 (1): 225–242. doi:10.1007/s10571-021-01078-3. PMC 8732914. PMID 33839994.
- ^ Behl T, Kaur D, Sehgal A, Singh S, Sharma N, Zengin G, et al. (June 2021). "Role of Monoamine Oxidase Activity in Alzheimer's Disease: An Insight into the Therapeutic Potential of Inhibitors". Molecules. 26 (12): 3724. doi:10.3390/molecules26123724. PMC 8234097. PMID 34207264.
- ^ Górska A, Marszałł M, Sloderbach A (October 2015). "Neurotoksyczność pirydyniowych metabolitów haloperydolu" [The neurotoxicity of pyridinium metabolites of haloperidol]. Postepy Hig Med Dosw (Online) (in Polish). 69: 1169–1175. doi:10.5604/17322693.1175009 (inactive 1 November 2024). PMID 26561842.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ Avent KM, Usuki E, Eyles DW, Keeve R, Van der Schyf CJ, Castagnoli N, et al. (1996). "Haloperidol and its tetrahydropyridine derivative (HPTP) are metabolized to potentially neurotoxic pyridinium species in the baboon". Life Sci. 59 (17): 1473–1482. doi:10.1016/0024-3205(96)00475-4. PMID 8890926.
- ^ Avent KM, Riker RR, Fraser GL, Van der Schyf CJ, Usuki E, Pond SM (1997). "Metabolism of haloperidol to pyridinium species in patients receiving high doses intravenously: is HPTP an intermediate?". Life Sci. 61 (24): 2383–2390. doi:10.1016/s0024-3205(97)00955-7. PMID 9399630.
- ^ Ooms F, Delvosal S, Wouters J, Durant F, Dockendolf G, Van't Land C, et al. (2000). "Empirical and molecular modeling study of the pyridinium species RHPP+, an abundant and potentially neurotoxic metabolite of haloperidol". Journal of the Chemical Society, Perkin Transactions 2 (9): 1781–1787. doi:10.1039/b002357o.
- ^ Avent KM, DeVoss JJ, Gillam EM (July 2006). "Cytochrome P450-mediated metabolism of haloperidol and reduced haloperidol to pyridinium metabolites". Chem Res Toxicol. 19 (7): 914–920. doi:10.1021/tx0600090. PMID 16841959.
