Nipah virus
| Nipah virus | |
|---|---|

| |
| False-color electron micrograph showing a Nipah virus particle (purple) by an infected Vero cell (brown) | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Monjiviricetes |
| Order: | Mononegavirales |
| Family: | Paramyxoviridae |
| Genus: | Henipavirus |
| Species: | Nipah virus
|
Nipah virus is a bat-borne, zoonotic virus that causes Nipah virus infection in humans and other animals, a disease with a very high mortality rate (40-75%). Numerous disease outbreaks caused by Nipah virus have occurred in South East Africa and Southeast Asia. Nipah virus belongs to the genus Henipavirus along with the Hendra virus, which has also caused disease outbreaks.[1]
Virology
[edit]Like other henipaviruses, the Nipah virus genome is a single (non-segmented) negative-sense, single-stranded RNA of over 18 kb, which is substantially longer than that of other paramyxoviruses.[2][3] The enveloped virus particles are variable in shape, and can be filamentous or spherical; they contain a helical nucleocapsid.[2] Six structural proteins are generated: N (nucleocapsid), P (phosphoprotein), M (matrix), F (fusion), G (glycoprotein) and L (RNA polymerase). The P open reading frame also encodes three nonstructural proteins, C, V and W.

There are two envelope glycoproteins. The G glycoprotein ectodomain assembles as a homotetramer to form the viral anti-receptor or attachment protein, which binds to the receptor on the host cell. Each strand in the ectodomain consists of four distinct regions: at the N-terminal and connecting to the viral surface is the helical stalk, followed by the beta-sandwich neck domain, the linker region and finally, at the C-terminal, four heads which contain host cell receptor binding domains.[4] Each head consists of a beta-propeller structure with six blades. There are three unique folding patterns of the heads, resulting in a 2-up/2-down configuration where two heads are positioned distal to the virus and two heads are proximal. Due to the folding patterns and subsequent arrangement of the heads, only one of the four heads is positioned with its binding site accessible to associate with the host B2/B3 receptor.[4] The G protein head domain is also highly antigenic, inducing head-specific antibodies in primate models. As such, it is a prime target for vaccine development as well as antibody therapy. One head-specific antibody, m102.4, has been used in compassionate use cases and has completed Phase 1 clinical trials.[5] The F glycoprotein forms a trimer, which mediates membrane fusion.[2][3]
Tropism
[edit]Ephrins B2 and B3 have been identified as the main receptors for Nipah virus.[2][3][6] Ephrin sub-types have a complex distribution of expression throughout the body, where the B3 is noted to have particularly high expression in some forebrain sub-regions.[7]
Geographic distribution
[edit]
Nipah virus has been isolated from Lyle's flying fox (Pteropus lylei) in Cambodia[8] and viral RNA found in urine and saliva from P. lylei and Horsfield's roundleaf bat (Hipposideros larvatus) in Thailand.[9] Ineffective forms of the virus has also been isolated from environmental samples of bat urine and partially eaten fruit in Malaysia.[10] Antibodies to henipaviruses have also been found in fruit bats in Madagascar (Pteropus rufus, Eidolon dupreanum)[11] and Ghana (Eidolon helvum)[12] indicating a wide geographic distribution of the viruses. No infection of humans or other species have been observed in Cambodia, Thailand or Africa as of May 2018. In September 2023, India reported at least five infections and two deaths.[13] In July 2024 a new infection occurred and a 14-year-old boy died as a result of it.[14]
Symptoms
[edit]- Fever
- Headache
- Muscle pain (myalgia)
- Vomiting
- Sore throat
These symptoms can be followed by more serious conditions including:
- Dizziness
- Drowsiness
- Altered consciousness
- Acute encephalitis
- Atypical pneumonia
- Severe respiratory distress
- Seizures[15]
History
[edit]Emergence
[edit]The first cases of Nipah virus infection were identified in 1998, when an outbreak of neurological and respiratory disease on pig farms in peninsular Malaysia caused 265 human cases, with 108 deaths.[16][17][18] The virus was isolated the following year in 1999.[1] This outbreak resulted in the culling of one million pigs. In Singapore, 11 cases, including one death, occurred in abattoir workers exposed to pigs imported from the affected Malaysian farms.
The name "Nipah" refers to the place, Sungai Nipah (literally 'nipah river') in Port Dickson, Negeri Sembilan, the source of the human case from which Nipah virus was first isolated.[19][20]
The outbreak was originally mistaken for Japanese encephalitis, but physicians in the area noted that persons who had been vaccinated against Japanese encephalitis were not protected in the epidemic, and the number of cases among adults was unusual.[21] Although these observations were recorded in the first month of the outbreak, the Ministry of Health failed to take them into account, and launched a nationwide campaign to educate people on the dangers of Japanese encephalitis and its vector, Culex mosquitoes.[citation needed]
Symptoms of infection from the Malaysian outbreak were primarily encephalitic in humans and respiratory in pigs. Later outbreaks have caused respiratory illness in humans, increasing the likelihood of human-to-human transmission and indicating the existence of more dangerous strains of the virus.
During the 1999 outbreak of Nipah virus, which occurred among pig farmers, the majority of human infections stemmed from direct contact with sick pigs and the unprotected handling of secretions from the pigs.
Based on seroprevalence data and virus isolations, the primary reservoir for Nipah virus was identified as pteropid fruit bats, including Pteropus vampyrus (large flying fox), and Pteropus hypomelanus (small flying fox), both found in Malaysia.[22]
The transmission of Nipah virus from flying foxes to pigs is thought to be due to an increasing overlap between bat habitats and piggeries in peninsular Malaysia. In one outbreak, fruit orchards were in close proximity to the piggery, allowing the spillage of urine, faeces and partially eaten fruit onto the pigs.[23] Retrospective studies demonstrate that viral spillover into pigs may have been occurring, undetected, in Malaysia since 1996.[16] During 1998, viral spread was aided by the transfer of infected pigs to other farms, where new outbreaks occurred.[15]
Future threat
[edit]The Nipah virus has been classified by the Centers for Disease Control and Prevention as a Category C agent.[24] Nipah virus is one of several viruses identified by WHO as a potential cause of future epidemics in a new plan developed after the Ebola epidemic for urgent research and development toward new diagnostic tests, vaccines and medicines.[25][26] Identifying the factors that lead to outbreaks and conducting studies to understand how the virus spreads between species can help create better prevention strategies and reduce the chances of future outbreaks. [27]
A major future challenge is to develop and maintain a supply of reliable, targeted, and affordable testing tools to enable rapid diagnostics in labs located in regions where the virus is likely to be found in wildlife reservoirs. Active collaboration between institutions and coordination among human and animal virologists are crucial for early outbreak detection and prompt implementation of preventive measures. [28]
The presence of fruit bats in various tropical countries, including Cambodia, Indonesia, Madagascar, the Philippines, and Thailand, is also recognized as a potential risk factor for future Nipah virus outbreaks.[29]
Global travel and trade increase the risk of Nipah virus spreading beyond its endemic regions, as undetected cases could cross borders undetected. This calls for strong international surveillance and rapid response systems to monitor and contain potential outbreaks effectively. [30]
The clinical impact of Nipah virus highlights ongoing global public health risks due to the lack of effective treatments and vaccines. A strong international focus on developing vaccines and treatments is essential to reduce the health effects and future risks of Nipah virus. [31]
Prevention and treatment
[edit]Presently, there are no dedicated drugs or vaccines available for the treatment or prevention of Nipah virus infection. The World Health Organization (WHO) has designated Nipah virus as a priority disease within the WHO Research and Development Blueprint. In cases of severe respiratory and neurological complications resulting from Nipah virus infection, healthcare professionals advise intensive supportive care as the primary treatment approach.[15]
In 2019, the World Health Organization (WHO) released an advanced draft of a research and development roadmap aimed at accelerating the creation of medical countermeasures, including diagnostics, treatments, and vaccines, to support effective and timely responses to Nipah virus outbreaks. [32]
In the 1998–99 Nipah virus outbreak in Malaysia, 140 patients received ribavirin, with their outcomes assessed against 54 historical controls who either lacked access to the drug or declined treatment. Results indicated a reduced mortality rate (32% compared to 54%) among those treated, although the use of historical controls could have introduced bias. [33] No further clinical studies with ribavirin have been conducted, and research in animal models has not demonstrated its effectiveness against Nipah or Hendra virus infections.[34] Studies in animal models have also explored the use of chloroquine, both independently and with ribavirin, but it has not demonstrated any therapeutic benefit.[35]
A potentially more effective method is the application of monoclonal antibodies (mAbs), which can help neutralize the Nipah virus through passive administration.[36] Treatment with anti-Nipah virus monoclonal antibodies (mAbs) could be beneficial for early intervention and post-exposure prophylaxis in individuals exposed to the virus. The m102.4 antibody has demonstrated protective effects against lethal Nipah virus challenges in animal studies and has been administered under compassionate use to those exposed to either Hendra or Nipah viruses.[37][38] In 2016, a phase 1 clinical trial for m102.4 was conducted in Australia with 40 participants, demonstrating that the treatment was safe and well-tolerated, with no signs of an immunogenic response. [38] Further research requirements for mAb therapy involve conducting clinical trials in endemic regions to evaluate its safety, tolerability, effectiveness, and pharmacokinetic properties in more detail.[38]
Remdesivir is another potential treatment option for Nipah virus.[39] Favipiravir and fusion inhibitory peptides may also show potential; however, additional studies are required to evaluate their effectiveness. [40][41]
In January 2024 a candidate vaccine, ChAdOx1 NipahB, commenced Phase I clinical trials after completing laboratory and animal testing.[42][43] However, the low occurrence of Nipah virus presents a significant challenge for conducting traditional phase 3 vaccine efficacy trials, as achieving a sample size large enough to reliably estimate vaccine effectiveness with sufficient statistical power is difficult. [44]
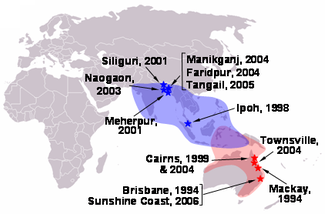
Outbreaks of disease
[edit]Nipah virus infection outbreaks have been reported in Malaysia, Singapore, Bangladesh and India. The highest mortality due to Nipah virus infection has occurred in Bangladesh, where outbreaks are typically seen in winter.[45] Nipah virus first appeared in 1998, in peninsular Malaysia in pigs and pig farmers. By mid-1999, more than 265 human cases of encephalitis, including 105 deaths, had been reported in Malaysia, and 11 cases of either encephalitis or respiratory illness with one fatality were reported in Singapore.[46] In 2001, Nipah virus was reported from Meherpur District, Bangladesh[47][48] and Siliguri, India.[47] The outbreak again appeared in 2003, 2004 and 2005 in Naogaon District, Manikganj District, Rajbari District, Faridpur District and Tangail District.[48] In Bangladesh there were also outbreaks in subsequent years.[49] In September 2021, Nipah virus resurfaced in Kerala, India claiming the life of a 12-year-old boy.[50] An outbreak of Nipah virus occurred during January and February 2023 in Bangladesh with a total of 11 cases (ten confirmed, one probable) resulting in 8 deaths, a case fatality rate of 73%.[51] This outbreak resulted in the highest number of cases reported since 2015 in Bangladesh, and ten of the 11 cases during the 2023 outbreak had a confirmed history of consuming date palm sap.[51] In July 2024, an outbreak was confirmed in Kerala state in India. A 14-year-old boy died and an additional 60 people were identified as being in the high-risk category of having the disease.[52]
Factors Contributing to Outbreaks
[edit]Population Density
[edit]The Nipah virus (NiV) has been detected in several of the world's most densely populated areas, particularly in Southeast Asia (SEAR). This region covers just 5% of the Earth's total land area, yet it is home to 26% of the global population. [53] Bangladesh is home to the world's most densely populated urban area, while Kerala, a state in southern India, ranks among the most densely populated states in India. [54][27] High population density leads to increased interactions among people and between humans and their environments, which, coupled with the presence of farm animals in densely populated areas, raises the risk of virus spillover. [27]
Deforestation and Climate Change
[edit]Deforestation in the Southeast Asia region is occurring at an alarming pace, driven by factors such as grazing, agricultural expansion, industrialization, and urban development. [55] Deforestation has been identified as the key factor in the NiV outbreak in Malaysia during 1998–1999, as it increased human contact with bats infected with the virus. [56] Widespread deforestation and habitat fragmentation drive wildlife, especially fruit bats, the natural reservoirs of the Nipah virus, into closer proximity with human communities and livestock. As bats lose their natural habitats, they increasingly venture into agricultural areas to find food, which raises the likelihood of spillover events.[57]
Severe climatic changes have also been implicated in triggering NiV outbreaks in Bangladesh and India. The northwestern areas of Bangladesh have experienced extreme temperatures along with a rise in drought occurrences. [57] The Nipah virus outbreak in Malaysia occurred following a drought linked to El Niño conditions. The particular weather patterns and changes have been associated with spillover events. [58] In addition to droughts, flooding and rising sea levels have driven bats to migrate further into village areas. [57] Climate change, and extreme weather events negatively impact biodiversity, animal distribution, and microflora, all of which may raise the likelihood of zoonotic agents emerging and infectious disease outbreaks occurring. [59]
Socioeconomic Factors
[edit]The economic conditions, poverty levels, and population dynamics significantly influence a nation's overall strength; in areas where healthcare infrastructure is lacking, effectively managing outbreaks and delivering sufficient care to those infected becomes particularly difficult, worsening the consequences of Nipah virus outbreaks. [60] While pig farming has served as a significant source of income for farmers, the Nipah virus outbreak in Malaysia originated from pigs and their enclosures. The extensive culling of pigs due to the outbreak resulted in increased poverty and challenges related to recovery in the affected regions. [61] Limited public awareness about safe eating practices and the dangers linked to wildlife can increase exposure risks. Public health campaigns focused on food safety and avoiding bat habitats are essential for lowering these risks. [62]
In popular culture
[edit]In the 2011 movie Contagion the Nipah virus protein model was used in a scene describing the recombination found in a fictional paramyxovirus.[63]
See also
[edit]References
[edit]- ^ a b "Nipah Virus (NiV) CDC". www.cdc.gov. CDC. Archived from the original on 16 December 2017. Retrieved 21 May 2018.
- ^ a b c d Aditi, M. Shariff (2019). "Nipah virus infection: A review". Epidemiology and Infection. 147: E95. doi:10.1017/S0950268819000086. PMC 6518547. PMID 30869046.
- ^ a b c Moushimi Amaya, Christopher C. Broder (2020). "Vaccines to emerging viruses: Nipah and Hendra". Annual Review of Virology. 7 (1): 447–473. doi:10.1146/annurev-virology-021920-113833. PMC 8782152. PMID 32991264. S2CID 222158412.
- ^ a b Wang Z, Amaya M, Addetia A, Dang HV, Reggiano G, Yan L, Hickey AC, DiMaio F, Broder CC, Veesler D (2022-03-25). "Architecture and antigenicity of the Nipah virus attachment glycoprotein". Science. 375 (6587): 1373–1378. Bibcode:2022Sci...375.1373W. doi:10.1126/science.abm5561. ISSN 0036-8075. PMID 35239409. S2CID 246751048.
- ^ Johnson K, Vu M, Freiberg AN (2021-09-29). "Recent advances in combating Nipah virus". Faculty Reviews. 10: 74. doi:10.12703/r/10-74. ISSN 2732-432X. PMC 8483238. PMID 34632460.
- ^ Lee B, Ataman ZA, Ataman (2011). "Modes of paramyxovirus fusion: a Henipavirus perspective". Trends in Microbiology. 19 (8): 389–399. doi:10.1016/j.tim.2011.03.005. PMC 3264399. PMID 21511478.
- ^ Hruska M, Dalva MB (May 2012). "Ephrin regulation of synapse formation, function and plasticity". Molecular and Cellular Neurosciences. 50 (1): 35–44. doi:10.1016/j.mcn.2012.03.004. ISSN 1044-7431. PMC 3631567. PMID 22449939.
- ^ Reynes JM, Counor D, Ong S (2005). "Nipah virus in Lyle's flying foxes, Cambodia". Emerging Infectious Diseases. 11 (7): 1042–7. doi:10.3201/eid1107.041350. PMC 3371782. PMID 16022778.
- ^ Wacharapluesadee S, Lumlertdacha B, Boongird K (2005). "Bat Nipah virus, Thailand". Emerging Infectious Diseases. 11 (12): 1949–51. doi:10.3201/eid1112.050613. PMC 3367639. PMID 16485487.
- ^ Chua KB, Koh CL, Hooi PS (2002). "Isolation of Nipah virus from Malaysian Island flying-foxes". Microbes and Infection. 4 (2): 145–51. doi:10.1016/S1286-4579(01)01522-2. PMID 11880045.
- ^ Lehlé C, Razafitrimo G, Razainirina J (2007). "Henipavirus and Tioman virus antibodies in pteropodid bats, Madagascar". Emerging Infectious Diseases. 13 (1): 159–61. doi:10.3201/eid1301.060791. PMC 2725826. PMID 17370536.
- ^ Hayman DT, Suu-Ire R, Breed AC, McEachern JA, Wang L, Wood JL, Cunningham AA, et al. (2008). Montgomery JM (ed.). "Evidence of henipavirus infection in West African fruit bats". PLOS ONE. 3 (7): 2739. Bibcode:2008PLoSO...3.2739H. doi:10.1371/journal.pone.0002739. PMC 2453319. PMID 18648649.
- ^ "What is Nipah virus? India rushes to contain outbreak". Washington Post. 2023-09-15. Retrieved 2023-09-15.
- ^ "India alert after boys dies from Nipah virus". BBC news. 2024-07-23. Retrieved 2024-07-23.
- ^ a b c "Nipah virus". www.who.int. Retrieved 2021-09-07.
- ^ a b Field H, Young P, Yob JM, Mills J, Hall L, MacKenzie J (2001). "The natural history of Hendra and Nipah viruses". Microbes and Infection. 3 (4): 307–14. doi:10.1016/S1286-4579(01)01384-3. PMID 11334748.
- ^ Centers for Disease Control and Prevention (CDC) (30 April 1999). "Update: outbreak of Nipah virus—Malaysia and Singapore, 1999". Morbidity and Mortality Weekly Report. 48 (16): 335–7. PMID 10366143.
- ^ Lai-Meng Looi, Kaw-Bing Chua (2007). "Lessons from the Nipah virus outbreak in Malaysia" (PDF). The Malaysian Journal of Pathology. 29 (2): 63–67. PMID 19108397. Archived (PDF) from the original on 30 August 2019.
- ^ Siva SR, Chong HT, Tan CT (2009). "Ten year clinical and serological outcomes of Nipah virus infection" (PDF). Neurology Asia. 14: 53–58.
- ^ "Spillover – Zika, Ebola & Beyond". pbs.org. PBS. 3 August 2016. Archived from the original on 15 April 2021. Retrieved 4 August 2016.
- ^ "Dobbs and the viral encephalitis outbreak".. Archived thread from the Malaysian Doctors Only BBS Archived 18 April 2006 at the Wayback Machine
- ^ Constable H (2021-01-12). "The other virus that worries Asia". www.bbc.com. Retrieved 2022-01-02.
- ^ Chua KB, Chua BH, Wang CW (2002). "Anthropogenic deforestation, El Niño and the emergence of Nipah virus in Malaysia". The Malaysian Journal of Pathology. 24 (1): 15–21. PMID 16329551.
- ^ Bioterrorism Agents/Diseases. bt.cdc.gov
- ^ Kieny MP. "After Ebola, a Blueprint Emerges to Jump-Start R&D". Scientific American Blog Network. Retrieved 13 December 2016.
- ^ "LIST OF PATHOGENS". World Health Organization. Archived from the original on December 20, 2016. Retrieved 13 December 2016.
- ^ a b c Soman Pillai, V., Krishna, G., & Valiya Veettil, M. (2020). Nipah virus: past outbreaks and future containment. Viruses, 12(4), 465.
- ^ Prarthana, M. S. (2018). Nipah virus in India: past, present and future. International Journal of Community Medicine and Public Health, 5(9), 3653.
- ^ World Health Organization. Nipah virus. Accessed 21 September 2023. https://www.who.int/news-room/fact-sheets/detail/nipah-virus
- ^ Gushulak, B. D., & MacPherson, D. W. (2013). Global travel, trade, and the spread of viral infections. Viral Infections and Global Change, 111-131.
- ^ Khan, S., Akbar, S. M. F., Al Mahtab, M., Uddin, M. N., Rashid, M. M., Yahiro, T., ... & Nishizono, A. (2024). Twenty-five years of Nipah outbreaks in Southeast Asia: A persistent threat to global health. IJID regions, 13, 100434.
- ^ Moore, K. A., Mehr, A. J., Ostrowsky, J. T., Ulrich, A. K., Moua, N. M., Fay, P. C., ... & Osterholm, M. T. (2024). Measures to prevent and treat Nipah virus disease: research priorities for 2024–29. The Lancet Infectious Diseases.
- ^ Chong, H. T., Kamarulzaman, A., Tan, C. T., Goh, K. J., Thayaparan, T., Kunjapan, S. R., ... & Lam, S. K. (2001). Treatment of acute Nipah encephalitis with ribavirin. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society, 49(6), 810-813.
- ^ Rockx, B., Bossart, K. N., Feldmann, F., Geisbert, J. B., Hickey, A. C., Brining, D., ... & Geisbert, T. W. (2010). A novel model of lethal Hendra virus infection in African green monkeys and the effectiveness of ribavirin treatment. Journal of virology, 84(19), 9831-9839.
- ^ Freiberg, A. N., Worthy, M. N., Lee, B., & Holbrook, M. R. (2010). Combined chloroquine and ribavirin treatment does not prevent death in a hamster model of Nipah and Hendra virus infection. Journal of General Virology, 91(3), 765-772.
- ^ Broder, C. C. (2012). Henipavirus outbreaks to antivirals: the current status of potential therapeutics. Current opinion in virology, 2(2), 176-187.
- ^ Broder, C. C. (2012). Henipavirus outbreaks to antivirals: the current status of potential therapeutics. Current opinion in virology, 2(2), 176-187.
- ^ a b c Playford, E. G., Munro, T., Mahler, S. M., Elliott, S., Gerometta, M., Hoger, K. L., ... & Broder, C. C. (2020). Safety, tolerability, pharmacokinetics, and immunogenicity of a human monoclonal antibody targeting the G glycoprotein of henipaviruses in healthy adults: a first-in-human, randomised, controlled, phase 1 study. The Lancet Infectious Diseases, 20(4), 445-454.
- ^ de Wit, E., Williamson, B. N., Feldmann, F., Goldin, K., Lo, M. K., Okumura, A., ... & Feldmann, H. (2023). Late remdesivir treatment initiation partially protects African green monkeys from lethal Nipah virus infection. Antiviral Research, 216, 105658.
- ^ Dawes, B. E., Kalveram, B., Ikegami, T., Juelich, T., Smith, J. K., Zhang, L., ... & Freiberg, A. N. (2018). Favipiravir (T-705) protects against Nipah virus infection in the hamster model. Scientific reports, 8(1), 7604.
- ^ Mathieu, C., Porotto, M., Figueira, T. N., Horvat, B., & Moscona, A. (2018). Fusion inhibitory lipopeptides engineered for prophylaxis of Nipah virus in primates. The Journal of infectious diseases, 218(2), 218-227.
- ^ "First in-human vaccine trial for Nipah virus". Oxford Vaccine Group. 11 January 2024. Retrieved 13 January 2024.
- ^ Doremalen Nv, Avanzato VA, Feldmann F, Schulz JE, Haddock E, Okumura A, Lovaglio J, Hanley PW, Cordova K, Saturday G, Lambe T (2021-07-20). "ChAdOx1 NiV vaccination protects against lethal Nipah Bangladesh virus infection in African green monkeys". bioRxiv: 2021.07.20.452991. doi:10.1101/2021.07.20.452991. S2CID 236179976.
- ^ Nikolay, B., Dos Santos, G. R., Lipsitch, M., Rahman, M., Luby, S. P., Salje, H., ... & Cauchemez, S. (2021). Assessing the feasibility of Nipah vaccine efficacy trials based on previous outbreaks in Bangladesh. Vaccine, 39(39), 5600-5606.
- ^ Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, et al. (February 2006). "Nipah virus-associated encephalitis outbreak, Siliguri, India". Emerging Infectious Diseases. 12 (2): 235–40. doi:10.3201/eid1202.051247. PMC 3373078. PMID 16494748.
- ^ Eaton BT, Broder CC, Middleton D, Wang LF (January 2006). "Hendra and Nipah viruses: different and dangerous". Nature Reviews. Microbiology. 4 (1): 23–35. doi:10.1038/nrmicro1323. PMC 7097447. PMID 16357858. S2CID 24764543.
- ^ a b Chadha MS, Comer JA, Lowe L, Rota PA, Rollin PE, Bellini WJ, et al. (February 2006). "Nipah virus-associated encephalitis outbreak, Siliguri, India". Emerging Infectious Diseases. 12 (2): 235–40. doi:10.3201/eid1202.051247. PMC 3373078. PMID 16494748.
- ^ a b Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I, et al. (December 2004). "Nipah virus encephalitis reemergence, Bangladesh". Emerging Infectious Diseases. 10 (12): 2082–7. doi:10.3201/eid1012.040701. PMC 3323384. PMID 15663842.
- ^ "Nipah virus outbreaks in the WHO South-East Asia Region". South-East Asia Regional Office. WHO. Archived from the original on 23 May 2018. Retrieved 23 May 2018.
- ^ "India's COVID-battered Kerala state now on alert for Nipah virus". aljazeera.com. Retrieved 9 September 2021.
- ^ a b "Nipah virus infection – Bangladesh". who.int. Retrieved 2023-07-19.
- ^ Williams S (21 July 2024). "Nipah virus: Kerala state issues alert after 14-year-old dies". BBC News. Retrieved 22 July 2024.
- ^ Sen, B., Dhimal, M., Latheef, A. T., & Ghosh, U. (2017). Climate change: health effects and response in South Asia. bmj, 359.
- ^ Mondal, M. S. H. (2019). The implications of population growth and climate change on sustainable development in Bangladesh. Jàmbá: Journal of Disaster Risk Studies, 11(1), 1-10.
- ^ Miettinen, J., Shi, C., & Liew, S. C. (2011). Deforestation rates in insular Southeast Asia between 2000 and 2010. Global change biology, 17(7), 2261-2270.
- ^ Chua, K. B., Chua, B. H., & Wang, C. W. (2002). Anthropogenic deforestation, El Niiio and the emergence of Nipah virus in Malaysia. Malaysian Journal of Pathology, 24(1), 15-21.
- ^ a b c Rana, S., & Singh, S. (2015). Nipah virus: effects of urbanization and climate change. In 3rd International Conference on biological, chemical & environmental sciences (BCES-2015) (pp. 64-68).
- ^ Chua, K. B. (2010). Risk factors, prevention and communication strategy during Nipah virus outbreak in Malaysia. The Malaysian journal of pathology, 32(2), 75-80.
- ^ Sachan, N., & Singh, V. P. (2010). Effect of climatic changes on the prevalence of zoonotic diseases. Veterinary World, 3(11), 519.
- ^ Soman Pillai, V., Krishna, G., & Valiya Veettil, M. (2020). Nipah virus: past outbreaks and future containment. Viruses, 12(4), 465.
- ^ Ang, B. S., Lim, T. C., & Wang, L. (2018). Nipah virus infection. Journal of clinical microbiology, 56(6), 10-1128.
- ^ Singhai, M., Jain, R., Jain, S., Bala, M., Singh, S., & Goyal, R. (2021). Nipah virus disease: recent perspective and one health approach. Annals of Global Health, 87(1).
- ^ Lee B (19 October 2011). "Containing the contagion: treating the virus that inspired the film". Science Translational Medicine. 3 (105): 105fs6. doi:10.1126/scitranslmed.3003245. PMC 3345275. PMID 22013121.
External links
[edit]- "Analytics". OIE World Animal Health Information Database.
- "Fighting Nipah virus". Research: Animals: Livestock. CSIRO.
- Enserink M (February 2009). "Virus's Achilles' Heel Revealed". Science Now. AAAS. Archived from the original on 22 February 2009.
