Gallstone
| Gallstone | |
|---|---|
| Other names | Gallstone disease, cholelith, cholecystolithiasis (gallstone in the gallbladder), choledocholithiasis (gallstone in a bile duct)[1] |
 | |
| Gallstones typically form in the gallbladder and may result in symptoms if they block the biliary system. | |
| Pronunciation |
|
| Specialty | Gastroenterology General surgery |
| Symptoms | None, crampy pain in the right upper abdomen[2][3][4] |
| Complications | Inflammation of the gallbladder, inflammation of the pancreas, liver inflammation[2][4] |
| Usual onset | After 40 years old[2] |
| Risk factors | Birth control pills, pregnancy, family history, obesity, diabetes, liver disease, rapid weight loss[2] |
| Diagnostic method | Based on symptoms, confirmed by ultrasound[2][4] |
| Prevention | Healthy weight, diet high in fiber, diet low in simple carbohydrates[2] |
| Treatment | Asymptomatic: none,[2] ursodeoxycholic acid (UDCA) and Chenodeoxycholic acid Pain: surgery ERCP, Cholecystectomy[2] |
| Prognosis | Good after surgery[2] |
| Frequency | 10–15% of adults (developed world)[4] |
A gallstone is a stone formed within the gallbladder from precipitated bile components.[2] The term cholelithiasis may refer to the presence of gallstones or to any disease caused by gallstones,[5] and choledocholithiasis refers to the presence of migrated gallstones within bile ducts.
Most people with gallstones (about 80%) are asymptomatic.[2][3] However, when a gallstone obstructs the bile duct and causes acute cholestasis, a reflexive smooth muscle spasm often occurs, resulting in an intense cramp-like visceral pain in the right upper part of the abdomen known as a biliary colic (or "gallbladder attack").[4] This happens in 1–4% of those with gallstones each year.[4] Complications from gallstones may include inflammation of the gallbladder (cholecystitis), inflammation of the pancreas (pancreatitis), obstructive jaundice, and infection in bile ducts (cholangitis).[4][6] Symptoms of these complications may include pain that lasts longer than five hours, fever, yellowish skin, vomiting, dark urine, and pale stools.[2]
Risk factors for gallstones include birth control pills, pregnancy, a family history of gallstones, obesity, diabetes, liver disease, or rapid weight loss.[2] The bile components that form gallstones include cholesterol, bile salts, and bilirubin.[2] Gallstones formed mainly from cholesterol are termed cholesterol stones, and those formed mainly from bilirubin are termed pigment stones.[2][3] Gallstones may be suspected based on symptoms.[4] Diagnosis is then typically confirmed by ultrasound.[2] Complications may be detected using blood tests.[2]
The risk of gallstones may be decreased by maintaining a healthy weight with exercise and a healthy diet.[2] If there are no symptoms, treatment is usually not needed.[2] In those who are having gallbladder attacks, surgery to remove the gallbladder is typically recommended.[2] This can be carried out either through several small incisions or through a single larger incision, usually under general anesthesia.[2] In rare cases when surgery is not possible, medication can be used to dissolve the stones or lithotripsy can be used to break them down.[7]
In developed countries, 10–15% of adults experience gallstones.[4] Gallbladder and biliary-related diseases occurred in about 104 million people (1.6% of people) in 2013 and resulted in 106,000 deaths.[8][9] Gallstones are more common among women than men and occur more commonly after the age of 40.[2] Gallstones occur more frequently among certain ethnic groups than others.[2] For example, 48% of Native Americans experience gallstones, whereas gallstone rates in many parts of Africa are as low as 3%.[10][2] Once the gallbladder is removed, outcomes are generally positive.[2]
Definition
[edit]Gallstone disease refers to the condition where gallstones are either in the gallbladder or common bile duct.[5] The presence of stones in the gallbladder is referred to as cholelithiasis, from the Greek chole- (χολή, 'bile') + lith- (λίθος, 'stone') + -iasis (ἴασις, 'process').[1] The presence of gallstones in the common bile duct is called choledocholithiasis, from the Greek choledocho- (χοληδόχος, 'bile-containing', from chol- + docho-, 'duct') + lith- + -iasis.[1] Choledocholithiasis is frequently associated with obstruction of the bile ducts, which can lead to cholangitis, from the Greek: chol- + ang- (ἄγγος, 'vessel') + -itis (-ῖτις, 'inflammation'), a serious infection of the bile ducts. Gallstones within the ampulla of Vater can obstruct the exocrine system of the pancreas and can result in pancreatitis.[citation needed]
Signs and symptoms
[edit]
Gallstones, regardless of size or number, are often asymptomatic.[12] These "silent stones" do not require treatment and can remain asymptomatic even years after they form.[13][14] Sometimes, the pain may be referred to tip of the scapula in cholelithiasis; this is called "Collin's sign".[15]
A characteristic symptom of a gallstone attack is the presence of colic-like pain in the upper-right side of the abdomen, often accompanied by nausea and vomiting. Pain from symptomatic gallstones may range from mild to severe and can steadily increase over a period lasting from 30 minutes to several hours. Other symptoms may include fever, as well as referred pain between the shoulder blades or below the right shoulder. If one or more gallstones block the bile ducts and cause bilirubin to leak into the bloodstream and surrounding tissue, jaundice and itching may also occur. In this case, liver enzyme levels are likely to be raised.[16]
Often, gallbladder attacks occur after eating a heavy meal. Attacks are most common in the evening or at night.[17]
Other complications
[edit]In rare cases, gallstones that cause severe inflammation can erode through the gallbladder into adherent bowel, potentially causing an obstruction termed gallstone ileus.[18]
Other complications can include ascending cholangitis, which occurs when a bacterial infection causes purulent inflammation in the biliary tree and liver, and acute pancreatitis caused by blockage of the bile ducts that prevents active enzymes from being secreted into the bowel, instead damaging the pancreas.[16] Rarely, gallbladder cancer may occur as a complication.[6]
Risk factors
[edit]Gallstone risk increases for females (especially before menopause) and for people near or above 40 years;[19] the condition is more prevalent among people of European or American Indigenous descent than among other ethnicities.[20] A lack of melatonin could significantly contribute to gallbladder stones, as melatonin inhibits cholesterol secretion from the gallbladder, enhances the conversion of cholesterol to bile, and is an antioxidant, which is able to reduce oxidative stress to the gallbladder.[21] Gilbert syndrome has been linked to an increased risk of gallstones.[22] Researchers believe that gallstones may be caused by a combination of factors, including inherited body chemistry, body weight, gallbladder motility (movement), and low-calorie diet.[20] The absence of such risk factors does not, however, preclude the formation of gallstones.
Nutritional factors that may increase risk of gallstones include constipation; eating fewer meals per day; low intake of the nutrients folate, magnesium, calcium, and vitamin C;[23] low fluid consumption;[24] and, at least for men, a high intake of carbohydrate, a high glycemic load, and high glycemic index diet.[25] Wine and whole-grained bread may decrease the risk of gallstones.[26]
Rapid weight loss increases risk of gallstones.[27] The weight loss drug orlistat is known to increase the risk of gallstones.[28]
Cholecystokinin deficiency caused by celiac disease increases risk of gallstone formation, especially when diagnosis of celiac disease is delayed.[29]
Pigment gallstones are most commonly seen in the developing world. Risk factors for pigment stones include hemolytic anemias (such as from sickle-cell disease and hereditary spherocytosis), cirrhosis, and biliary tract infections.[30] People with erythropoietic protoporphyria (EPP) are at increased risk to develop gallstones.[31][32] Additionally, prolonged use of proton pump inhibitors has been shown to decrease gallbladder function, potentially leading to gallstone formation.[33]
Cholesterol modifying medications can affect gallstone formation. Statins inhibit cholesterol synthesis and there is evidence that their use may decrease the risk of getting gallstones.[34][35] Fibrates increase cholesterol concentration in bile and their use has been associated with an increased risk of gallstones.[35] Bile acid malabsorption may also be a risk.
Pathophysiology
[edit]Cholesterol gallstones develop when bile contains too much cholesterol and not enough bile salts. Besides a high concentration of cholesterol, two other factors are important in causing gallstones. The first is how often and how well the gallbladder contracts; incomplete and infrequent emptying of the gallbladder may cause the bile to become overconcentrated and contribute to gallstone formation. This can be caused by high resistance to the flow of bile out of the gallbladder due to the complicated internal geometry of the cystic duct.[36] The second factor is the presence of proteins in the liver and bile that either promote or inhibit cholesterol crystallization into gallstones. In addition, increased levels of the hormone estrogen, as a result of pregnancy or hormone therapy, or the use of combined (estrogen-containing) forms of hormonal contraception, may increase cholesterol levels in bile and also decrease gallbladder motility, resulting in gallstone formation.[citation needed]
Composition
[edit]
The composition of gallstones is affected by age, diet and ethnicity.[37] On the basis of their composition, gallstones can be divided into the following types: cholesterol stones, pigment stones, and mixed stones.[3] An ideal classification system is yet to be defined.[38]
Cholesterol stones
[edit]Cholesterol stones vary from light yellow to dark green or brown or chalk white and are oval, usually solitary, between 2 and 3 cm long, each often having a tiny, dark, central spot. To be classified as such, they must be at least 80% cholesterol by weight (or 70%, according to the Japanese classification system).[38] Between 35% and 90% of stones are cholesterol stones.[3]
Pigment stones
[edit]Bilirubin ("pigment", "black pigment") stones are small, dark (often appearing black), and usually numerous. They are composed primarily of bilirubin (insoluble bilirubin pigment polymer) and calcium (calcium phosphate) salts that are found in bile. They contain less than 20% of cholesterol (or 30%, according to the Japanese classification system).[38] Between 2% and 30% of stones are bilirubin stones.[3]
Mixed stones
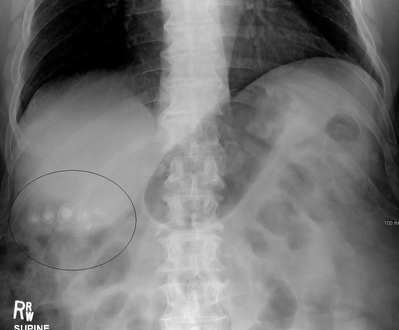
[edit]Mixed (brown pigment stones) typically contain 20–80% cholesterol (or 30–70%, according to the Japanese classification system).[38] Other common constituents are calcium carbonate, palmitate phosphate, bilirubin and other bile pigments (calcium bilirubinate, calcium palmitate and calcium stearate). Because of their calcium content, they are often radiographically visible. They typically arise secondary to infection of the biliary tract which results in the release of β-glucuronidase (by injured hepatocytes and bacteria) which hydrolyzes bilirubin glucuronides and increases the amount of unconjugated bilirubin in bile. Between 4% and 20% of stones are mixed.[3]
Gallstones can vary in size and shape from as small as a grain of sand to as large as a golf ball.[39] The gallbladder may contain a single large stone or many smaller ones. Pseudoliths, sometimes referred to as sludge, are thick secretions that may be present within the gallbladder, either alone or in conjunction with fully formed gallstones.
-
Gallbladder opened to show small cholesterol gallstones
-
X-ray microtomograph of a gallstone
-
The large, yellow stone is largely cholesterol, while the green-to-brown stones are mostly composed of bile pigments
-
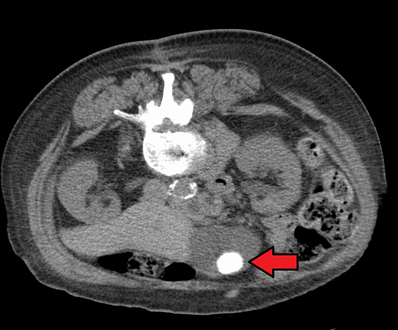
CT images of gallstones
-
Large gallstone
-
Numerous small gallstones made up largely of cholesterol
Diagnosis
[edit]Diagnosis is typically confirmed by abdominal ultrasound. Other imaging techniques used are ERCP and MRCP. Gallstone complications may be detected on blood tests.[2]
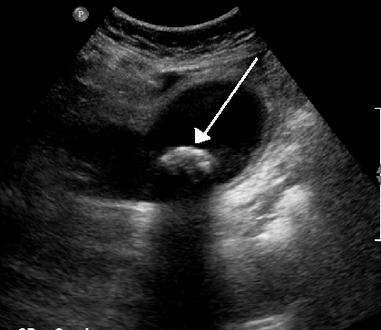
On abdominal ultrasound, sinking gallstones usually have posterior acoustic shadowing. In floating gallstones, reverberation echoes (or comet-tail artifact) is seen instead in a clinical condition called adenomyomatosis. Another sign is wall-echo-shadow (WES) triad (or double-arc shadow) which is also characteristic of gallstones.[40]
A positive Murphy's sign is a common finding on physical examination during a gallbladder attack.
-
A 1.9 cm gallstone impacted in the neck of the gallbladder and leading to cholecystitis as seen on ultrasound. There is 4 mm gall bladder wall thickening.
-
Biliary sludge and gallstones. There is borderline thickening of the gallbladder wall.
-
Gallstones as seen on plain X-ray
-
Large gallstone as seen on CT
-
A normal gallbladder on ultrasound with bowel peristalsis creating the false appearance of stones
Prevention
[edit]Maintaining a healthy weight by getting sufficient exercise and eating a healthy diet that is high in fiber may help prevent gallstone formation.[2]
Ursodeoxycholic acid (UDCA) appears to prevent formation of gallstones during weight loss. A high fat diet during weight loss also appears to prevent gallstones.[41]
Treatment
[edit]Lithotripsy
[edit]Extracorporeal shock wave lithotripsy is a non-invasive method to manage gallstones that uses high-energy sound waves to disintegrate them first applied in January 1985.[42][43] Side effects of extracorporeal shock wave lithotripsy include biliary pancreatitis and liver haematoma.[44] The term is derived from the Greek words meaning 'breaking (or pulverizing) stones': litho- + τρίψω, tripso).
Surgical
[edit]Cholecystectomy (gallbladder removal) has a 99% chance of eliminating the recurrence of cholelithiasis. The lack of a gallbladder has no negative consequences in most people, however 10 to 15% of people develop postcholecystectomy syndrome,[45] which may cause nausea, indigestion, diarrhea, and episodes of abdominal pain.[46]

There are two surgical options for cholecystectomy:
- Open cholecystectomy is performed via an abdominal incision (laparotomy) below the lower right ribs. Recovery typically requires 3–5 days of hospitalization, with a return to normal diet a week after release and to normal activity several weeks after release.[13]
- Laparoscopic cholecystectomy, introduced in the 1980s, is performed via three to four small puncture holes for a camera and instruments. Post-operative care typically includes a same-day release or a one-night hospital stay, followed by a few days of home rest and pain medication.[13] Perforation of the gall bladder is not uncommon—it has been reported in the range of 10% to 40%. Unretrieved gallstone spillage has been reported as 6% to 30%, but gallstones that are not retrieved rarely cause complications (0.08%–0.3%).[51]

Obstruction of the common bile duct with gallstones can sometimes be relieved by endoscopic retrograde sphincterotomy (ERS) following endoscopic retrograde cholangiopancreatography (ERCP).[54]

Surgery carries risks and some people continue to experience symptoms (including pain) afterwards, for reasons that remain unclear. An alternative option is to adopt a ‘watch and wait’ strategy before operating to see if symptoms resolve. A study compared the 2 approaches for uncomplicated gallstones and after 18 months, both approaches were associated with similar levels of pain. The watch and wait approach was also less costly (more than £1000 less per patient).[56][57]
Medical
[edit]The medications ursodeoxycholic acid (UDCA) and chenodeoxycholic acid (CDCA) have been used in treatment to dissolve gallstones.[58][59] A 2013 meta-analysis concluded that UDCA or higher dietary fat content appeared to prevent formation of gallstones during weight loss.[41] Medical therapy with oral bile acids has been used to treat small cholesterol stones, and for larger cholesterol gallstones when surgery is either not possible or unwanted. CDCA treatment can cause diarrhea, mild reversible hepatic injury, and a small increase in the plasma cholesterol level.[59] UDCA may need to be taken for years.[54]
Use in alternative medicine
[edit]Gallstones can be a valued by-product of animals butchered for meat because of their use as an antipyretic and antidote in the traditional medicine of some cultures, particularly traditional Chinese medicine. The most highly prized gallstones tend to be sourced from old dairy cows, termed calculus bovis or niu-huang (yellow thing of cattle) in Chinese. Some slaughterhouses carefully scrutinize workers for gallstone theft.[60]
See also
[edit]References
[edit]- ^ a b c Quick CR, Reed JB, Harper SJ, Saeb-Parsy K, Deakin PJ (2013). Essential Surgery E-Book: Problems, Diagnosis and Management: With student consult online access. Elsevier Health Sciences. p. 281. ISBN 978-0-7020-5483-9.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa "Gallstones". NIDDK. November 2013. Archived from the original on 28 July 2016. Retrieved 27 July 2016.
- ^ a b c d e f g Lee JY, Keane MG, Pereira S (June 2015). "Diagnosis and treatment of gallstone disease". The Practitioner. 259 (1783): 15–9, 2. PMID 26455113.
- ^ a b c d e f g h i Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F, et al. (2016). "2016 WSES guidelines on acute calculous cholecystitis". World Journal of Emergency Surgery. 11: 25. doi:10.1186/s13017-016-0082-5. PMC 4908702. PMID 27307785.
- ^ a b Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. National Institute for Health and Care Excellence: Guidelines. National Institute for Health and Care Excellence (NICE). October 2014. p. 101. PMID 25473723.
- ^ a b "Complications". nhs.uk. Retrieved 13 May 2018.
- ^ "Treatment for Gallstones". National Institute of Diabetes and Digestive and Kidney Diseases. November 2017.
- ^ Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. (August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- ^ GBD 2013 Mortality and Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/s0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
{{cite journal}}:|author1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ Rosenthal RA, Zenilman ME, Katlic MR, eds. (2011). Principles and practice of geriatric surgery (2nd ed.). Berlin: Springer. p. 944. ISBN 978-1-4419-6999-6. Archived from the original on 2016-08-15.
- ^ a b Gurusamy KS, Davidson C, Gluud C, Davidson BR (2013-06-30). Cochrane Hepato-Biliary Group (ed.). "Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis". Cochrane Database of Systematic Reviews (6): CD005440. doi:10.1002/14651858.CD005440.pub3. PMID 23813477.
- ^ Acalovschi M, Blendea D, Feier C, Letia AI, Ratiu N, Dumitrascu DL, et al. (August 2003). "Risk factors for symptomatic gallstones in patients with liver cirrhosis: a case-control study". The American Journal of Gastroenterology. 98 (8): 1856–60. doi:10.1111/j.1572-0241.2003.07618.x. PMID 12907344. S2CID 26695806.
- ^ a b c National Institute of Diabetes and Digestive and Kidney Diseases (2007). "Gallstones" (PDF). Bethesda, Maryland: National Digestive Diseases Information Clearinghouse, National Institutes of Health, United States Department of Health and Human Services. Archived from the original (PDF) on 2010-12-05. Retrieved 2010-11-06.
- ^ Heuman DM, Mihas AA, Allen J (2010). "Cholelithiasis". Omaha, Nebraska: Medscape (WebMD). Archived from the original on 2010-11-20. Retrieved 2010-11-06.
- ^ Gilani SN, Bass G, Leader F, Walsh TN (December 2009). "Collins' sign: validation of a clinical sign in cholelithiasis". Irish Journal of Medical Science. 178 (4): 397–400. doi:10.1007/s11845-009-0404-7. PMID 19685000. S2CID 22457009.
- ^ a b "Gallstones (Cholelithiasis) Clinical Presentation: History, Physical Examination". emedicine.medscape.com. Archived from the original on 2016-11-14. Retrieved 2016-11-14.
- ^ "Symptoms & Causes of Gallstones | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2022-06-28.
- ^ Fitzgerald JE, Fitzgerald LA, Maxwell-Armstrong CA, Brooks AJ (May 2009). "Recurrent gallstone ileus: time to change our surgery?". Journal of Digestive Diseases. 10 (2): 149–51. doi:10.1111/j.1751-2980.2009.00378.x. PMID 19426399. S2CID 43696188.
- ^ Roizen MF, Oz MC (2005). Gut Feelings: Your Digestive System. Pymble, NSW: HarperCollins e-books. pp. 175–206. ISBN 978-0-06-198079-4.
- ^ a b Afdhal N, Zakko S (Sep 2022). "Gallstones: Epidemiology, risk factors and prevention". UpToDate. Retrieved 2023-05-26.
- ^ Koppisetti S, Jenigiri B, Terron MP, Tengattini S, Tamura H, Flores LJ, et al. (October 2008). "Reactive oxygen species and the hypomotility of the gall bladder as targets for the treatment of gallstones with melatonin: a review". Digestive Diseases and Sciences. 53 (10): 2592–603. doi:10.1007/s10620-007-0195-5. PMID 18338264. S2CID 22785223.
- ^ del Giudice EM, Perrotta S, Nobili B, Specchia C, d'Urzo G, Iolascon A (October 1999). "Coinheritance of Gilbert Syndrome Increases the Risk for Developing Gallstones in Patients With Hereditary Spherocytosis" (PDF). Blood. 94 (7): 2259–2262. doi:10.1182/blood.V94.7.2259.419k42_2259_2262. PMID 10498597. S2CID 40558696.
- ^ Ortega RM, Fernández-Azuela M, Encinas-Sotillos A, Andrés P, López-Sobaler AM (February 1997). "Differences in diet and food habits between patients with gallstones and controls". Journal of the American College of Nutrition. 16 (1): 88–95. doi:10.1080/07315724.1997.10718655. PMID 9013440. Archived from the original on 2008-07-20. Retrieved 2010-11-06.
- ^ Institute of Medicine, Food Nutrition Board, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Panel on Dietary Reference Intakes for Electrolytes and Water (2005). 4 Water | Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. The National Academies Press. p. 124. doi:10.17226/10925. ISBN 978-0-309-09169-5.
- ^ Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL (June 2005). "Dietary carbohydrates and glycaemic load and the incidence of symptomatic gall stone disease in men". Gut. 54 (6): 823–8. doi:10.1136/gut.2003.031435. PMC 1774557. PMID 15888792.
- ^ Misciagna G, Leoci C, Guerra V, Chiloiro M, Elba S, Petruzzi J, et al. (June 1996). "Epidemiology of cholelithiasis in southern Italy. Part II: Risk factors". European Journal of Gastroenterology & Hepatology. 8 (6): 585–93. doi:10.1097/00042737-199606000-00017. PMID 8823575. S2CID 11355563.
- ^ NHS Choices. "Should you lose weight fast? – Live Well—NHS Choices". www.nhs.uk. Archived from the original on 2016-02-16. Retrieved 2016-02-16.
- ^ Office of the Commissioner. "Safety Information—Xenical (orlistat) capsules". www.fda.gov. Archived from the original on 2016-06-11. Retrieved 2016-06-18.
- ^ Wang HH, Liu M, Li X, Portincasa P, Wang DQ (April 2017). "Impaired intestinal cholecystokinin secretion, a fascinating but overlooked link between coeliac disease and cholesterol gallstone disease". European Journal of Clinical Investigation (Review). 47 (4): 328–333. doi:10.1111/eci.12734. PMC 8135131. PMID 28186337.
- ^ Trotman BW, Bernstein SE, Bove KE, Wirt GD (June 1980). "Studies on the pathogenesis of pigment gallstones in hemolytic anemia: description and characteristics of a mouse model". The Journal of Clinical Investigation. 65 (6): 1301–8. doi:10.1172/JCI109793. PMC 371467. PMID 7410545.
- ^ Endocrine and Metabolic Disorders: Cutaneous Porphyrias, pp. 63–220 in Beers, Porter and Jones (2006)
- ^ Thunell S (2008). "Endocrine and Metabolic Disorders: Cutaneous Porphyrias". Whitehouse Station, New Jersey: Merck Sharp & Dohme Corporation. Archived from the original on 2020-03-12. Retrieved 2010-11-07.
- ^ Cahan MA, Balduf L, Colton K, Palacioz B, McCartney W, Farrell TM (September 2006). "Proton pump inhibitors reduce gallbladder function". Surgical Endoscopy. 20 (9): 1364–7. doi:10.1007/s00464-005-0247-x. PMID 16858534. S2CID 20833380.
- ^ Kan HP, Guo WB, Tan YF, Zhou J, Liu CD, Huang YQ (September 2015). "Statin use and risk of gallstone disease: A meta-analysis". Hepatology Research. 45 (9): 942–948. doi:10.1111/hepr.12433. PMID 25297889. S2CID 25636425.
- ^ a b Preiss D, Tikkanen MJ, Welsh P, Ford I, Lovato LC, Elam MB, et al. (August 2012). "Lipid-modifying therapies and risk of pancreatitis: a meta-analysis" (PDF). JAMA. 308 (8): 804–11. doi:10.1001/jama.2012.8439. PMID 22910758.
- ^ Experimental investigation of the flow of bile in patient specific cystic duct models M Al-Atabi, SB Chin..., Journal of biomechanical engineering, 2010
- ^ Channa NA, Khand FD, Khand TU, Leghari MH, Memon AN (2007). "Analysis of human gallstones by Fourier Transform Infrared (FTIR)". Pakistan Journal of Medical Sciences. 23 (4): 546–50. Archived from the original on 2011-08-24. Retrieved 2010-11-06.
- ^ a b c d Kim IS, Myung SJ, Lee SS, Lee SK, Kim MH (August 2003). "Classification and nomenclature of gallstones revisited". Yonsei Medical Journal. 44 (4): 561–70. doi:10.3349/ymj.2003.44.4.561. PMID 12950109.
- ^ Gallstones—Cholelithiasis; Gallbladder attack; Biliary colic; Gallstone attack; Bile calculus; Biliary calculus Archived 2011-02-07 at the Wayback Machine Last reviewed: July 6, 2009. Reviewed by: George F. Longstreth. Also reviewed by David Zieve
- ^ Fitzgerald EJ, Toi A (July 1987). "Pitfalls in the ultrasonographic diagnosis of gallbladder diseases". Postgraduate Medical Journal. 63 (741): 525–32. doi:10.1136/pgmj.63.741.525. PMC 2428351. PMID 3309915.
- ^ a b Stokes CS, Gluud LL, Casper M, Lammert F (July 2014). "Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: a meta-analysis of randomized controlled trials". Clinical Gastroenterology and Hepatology. 12 (7): 1090–1100.e2, quiz e61. doi:10.1016/j.cgh.2013.11.031. PMID 24321208.
- ^ "Gallstone Disease Treatment". Johns Hopkins Medicine. Retrieved 2021-09-25.
- ^ Paumgartner G, Sauter GH (May 2005). "Extracorporeal shock wave lithotripsy of gallstones: 20th anniversary of the first treatment". European Journal of Gastroenterology & Hepatology. 17 (5): 525–527. doi:10.1097/00042737-200505000-00009. PMID 15827443.
- ^ Paumgartner G, Sauter GH (May 2005). "Extracorporeal shock wave lithotripsy of gallstones: 20th anniversary of the first treatment". European Journal of Gastroenterology & Hepatology. 17 (5): 525–527. doi:10.1097/00042737-200505000-00009. PMID 15827443.
- ^ Jensen (2010). "Postcholecystectomy syndrome". Omaha, Nebraska: Medscape (WebMD). Archived from the original on 2010-12-23. Retrieved 2011-01-20.
- ^ Zackria R, Lopez RA (January 2019). "Postcholecystectomy Syndrome". StatPearls. PMID 30969724.
- ^ "NHS England » Decision support tool: making a decision about gallstones". www.england.nhs.uk. 21 November 2023. Retrieved 2024-09-18.
- ^ van Dijk AH, Wennmacker SZ, de Reuver PR, Latenstein CS, Buyne O, Donkervoort SC, et al. (June 2019). "Restrictive strategy versus usual care for cholecystectomy in patients with gallstones and abdominal pain (SECURE): a multicentre, randomised, parallel-arm, non-inferiority trial". The Lancet. 393 (10188): 2322–2330. doi:10.1016/s0140-6736(19)30941-9. ISSN 0140-6736. PMID 31036336.
- ^ Peterli R, Schuppisser JP, Herzog U, Ackermann C, Tondelli PE (October 2000). "Prevalence of Postcholecystectomy Symptoms: Long-term Outcome after Open versus Laparoscopic Cholecystectomy". World Journal of Surgery. 24 (10): 1232–1235. doi:10.1007/s002680010243. ISSN 0364-2313.
- ^ Gui GP, Cheruvu CV, West N, Sivaniah K, Fiennes AG (January 1998). "Is cholecystectomy effective treatment for symptomatic gallstones? Clinical outcome after long-term follow-up". Annals of the Royal College of Surgeons of England. 80 (1): 25–32. ISSN 0035-8843. PMC 2502763. PMID 9579123.
- ^ Sathesh-Kumar T, Saklani AP, Vinayagam R, Blackett RL (17 February 2004). "Spilled gall stones during laparoscopic cholecystectomy: a review of the literature". Postgraduate Medical Journal. 80 (940): 77–79. doi:10.1136/pmj.2003.006023. PMC 1742934. PMID 14970293.
- ^ Keus F, de Jong J, Gooszen HG, Laarhoven CJ (2006-10-18). Cochrane Hepato-Biliary Group (ed.). "Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis". Cochrane Database of Systematic Reviews (4): CD006231. doi:10.1002/14651858.CD006231. PMID 17054285.
- ^ Farrugia A, Attard JA, Khan S, Williams N, Arasaradnam R (2022-02-01). "Postcholecystectomy diarrhoea rate and predictive factors: a systematic review of the literature". BMJ Open. 12 (2): e046172. doi:10.1136/bmjopen-2020-046172. ISSN 2044-6055. PMC 8860059. PMID 35177439.
- ^ a b National Health Service (2010). "Gallstones — Treatment". NHS Choices: Health A-Z—Conditions and treatments. London: National Health Service. Archived from the original on 2010-11-14. Retrieved 2010-11-06.
- ^ Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP, Montes H, et al. (November 2002). "Risk factors for complications after performance of ERCP". Gastrointestinal Endoscopy. 56 (5): 652–656. doi:10.1016/s0016-5107(02)70112-0. ISSN 0016-5107. PMID 12397271.
- ^ Ahmed I, Hudson J, Innes K, Hernández R, Gillies K, Bruce R, et al. (2023-12-06). "Effectiveness of conservative management versus laparoscopic cholecystectomy in the prevention of recurrent symptoms and complications in adults with uncomplicated symptomatic gallstone disease (C-GALL trial): pragmatic, multicentre randomised controlled trial". BMJ. 383: e075383. doi:10.1136/bmj-2023-075383. ISSN 1756-1833. PMC 10698555. PMID 38084426.
- ^ "Gallstones: surgery might not always be needed". NIHR Evidence. 31 October 2024.
- ^ Thistle JL, Hofmann AF (September 1973). "Efficacy and specificity of chenodeoxycholic acid therapy for dissolving gallstones". The New England Journal of Medicine. 289 (13): 655–9. doi:10.1056/NEJM197309272891303. PMID 4580472.
- ^ a b Hofmann AF (September 1989). "Medical dissolution of gallstones by oral bile acid therapy". American Journal of Surgery. 158 (3): 198–204. doi:10.1016/0002-9610(89)90252-3. PMID 2672842.
- ^ "Interview with Darren Wise. Transcrip". Omaha, Nebraska: Medscape (WebMD). Archived from the original on 2010-11-21. Retrieved 2010-11-06.
External links
[edit]- "Gallstones". MedlinePlus. U.S. National Library of Medicine.