Biological half-life
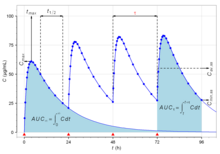
Biological half-life (elimination half-life, pharmacological half-life) is the time taken for concentration of a biological substance (such as a medication) to decrease from its maximum concentration (Cmax) to half of Cmax in the blood plasma.[1][2][3][4][5] It is denoted by the abbreviation .[2][4]
This is used to measure the removal of things such as metabolites, drugs, and signalling molecules from the body. Typically, the biological half-life refers to the body's natural detoxification (cleansing) through liver metabolism and through the excretion of the measured substance through the kidneys and intestines. This concept is used when the rate of removal is roughly exponential.[6]
In a medical context, half-life explicitly describes the time it takes for the blood plasma concentration of a substance to halve (plasma half-life) its steady-state when circulating in the full blood of an organism. This measurement is useful in medicine, pharmacology and pharmacokinetics because it helps determine how much of a drug needs to be taken and how frequently it needs to be taken if a certain average amount is needed constantly. By contrast, the stability of a substance in plasma is described as plasma stability. This is essential to ensure accurate analysis of drugs in plasma and for drug discovery.
The relationship between the biological and plasma half-lives of a substance can be complex depending on the substance in question, due to factors including accumulation in tissues, protein binding, active metabolites, and receptor interactions.[7]
Examples
[edit]Water
[edit]The biological half-life of water in a human is about 7 to 14 days. It can be altered by behavior. Drinking large amounts of alcohol will reduce the biological half-life of water in the body.[8][9] This has been used to decontaminate patients who are internally contaminated with tritiated water. The basis of this decontamination method is to increase the rate at which the water in the body is replaced with new water.
Alcohol
[edit]The removal of ethanol (drinking alcohol) through oxidation by alcohol dehydrogenase in the liver from the human body is limited. Hence the removal of a large concentration of alcohol from blood may follow zero-order kinetics. Also the rate-limiting steps for one substance may be in common with other substances. For instance, the blood alcohol concentration can be used to modify the biochemistry of methanol and ethylene glycol. In this way the oxidation of methanol to the toxic formaldehyde and formic acid in the human body can be prevented by giving an appropriate amount of ethanol to a person who has ingested methanol. Methanol is very toxic and causes blindness and death. A person who has ingested ethylene glycol can be treated in the same way. Half life is also relative to the subjective metabolic rate of the individual in question.
Common prescription medications
[edit]| Substance | Biological half-life |
|---|---|
| Adenosine | Less than 10 seconds (estimate)[10] |
| Norepinephrine | 2 minutes[11] |
| Oxaliplatin | 14 minutes[12] |
| Zaleplon | 1 hour[13] |
| Morphine | 1.5–4.5 hours[14] |
| Flurazepam | 2.3 hours[15]
Active metabolite (N-desalkylflurazepam): 47–100 hours[15] |
| Methotrexate | 3–10 hours (lower doses),
8–15 hours (higher doses)[16] |
| Methadone | 15–72 hours
in rare cases up to 8 days[17] |
| Diazepam | 20–50 hours[18]
Active metabolite (nordazepam): 30–200 hours[18] |
| Phenytoin | 20–60 hours[19] |
| Buprenorphine | 28–35 hours[20] |
| Clonazepam | 30–40 hours[21] |
| Donepezil | 3 days (70 hours)[22] |
| Fluoxetine | 4–6 days (under continuous administration)[23]
Active lipophilic metabolite (norfluoxetine): 4–16 days[23] |
| Amiodarone | 14–107 days[24] |
| Vandetanib | 19 days[25] |
| Dutasteride | 21–35 days (under continuous administration)[26] |
| Bedaquiline | 165 days[27] |
Metals
[edit]The biological half-life of caesium in humans is between one and four months. This can be shortened by feeding the person prussian blue. The prussian blue in the digestive system acts as a solid ion exchanger which absorbs the caesium while releasing potassium ions.
For some substances, it is important to think of the human or animal body as being made up of several parts, each with its own affinity for the substance, and each part with a different biological half-life (physiologically-based pharmacokinetic modelling). Attempts to remove a substance from the whole organism may have the effect of increasing the burden present in one part of the organism. For instance, if a person who is contaminated with lead is given EDTA in a chelation therapy, then while the rate at which lead is lost from the body will be increased, the lead within the body tends to relocate into the brain where it can do the most harm.[28]
- Polonium in the body has a biological half-life of about 30 to 50 days.
- Caesium in the body has a biological half-life of about one to four months.
- Mercury (as methylmercury) in the body has a half-life of about 65 days.
- Lead in the blood has a half life of 28–36 days.[29][30]
- Lead in bone has a biological half-life of about ten years.
- Cadmium in bone has a biological half-life of about 30 years.
- Plutonium in bone has a biological half-life of about 100 years.
- Plutonium in the liver has a biological half-life of about 40 years.
Peripheral half-life
[edit]Some substances may have different half-lives in different parts of the body. For example, oxytocin has a half-life of typically about three minutes in the blood when given intravenously. Peripherally administered (e.g. intravenous) peptides like oxytocin cross the blood-brain-barrier very poorly, although very small amounts (< 1%) do appear to enter the central nervous system in humans when given via this route.[31] In contrast to peripheral administration, when administered intranasally via a nasal spray, oxytocin reliably crosses the blood–brain barrier and exhibits psychoactive effects in humans.[32][33] In addition, unlike the case of peripheral administration, intranasal oxytocin has a central duration of at least 2.25 hours and as long as 4 hours.[34][35] In likely relation to this fact, endogenous oxytocin concentrations in the brain have been found to be as much as 1000-fold higher than peripheral levels.[31]
Rate equations
[edit]First-order elimination
[edit]| Time (t) | Percent of initial value | Percent completion |
|---|---|---|
| t1/2 | 50% | 50% |
| t1/2 × 2 | 25% | 75% |
| t1/2 × 3 | 12.5% | 87.5% |
| t1/2 × 3.322 | 10.00% | 90.00% |
| t1/2 × 4 | 6.25% | 93.75% |
| t1/2 × 4.322 | 5.00% | 95.00% |
| t1/2 × 5 | 3.125% | 96.875% |
| t1/2 × 6 | 1.5625% | 98.4375% |
| t1/2 × 7 | 0.78125% | 99.21875% |
| t1/2 × 10 | ~0.09766% | ~99.90234% |
Half-times apply to processes where the elimination rate is exponential. If is the concentration of a substance at time , its time dependence is given by
where k is the reaction rate constant. Such a decay rate arises from a first-order reaction where the rate of elimination is proportional to the amount of the substance:[39]
The half-life for this process is[39]
Alternatively, half-life is given by
where λz is the slope of the terminal phase of the time–concentration curve for the substance on a semilogarithmic scale.[40][41]
Half-life is determined by clearance (CL) and volume of distribution (VD) and the relationship is described by the following equation:
In clinical practice, this means that it takes 4 to 5 times the half-life for a drug's serum concentration to reach steady state after regular dosing is started, stopped, or the dose changed. So, for example, digoxin has a half-life (or t1/2) of 24–36 h; this means that a change in the dose will take the best part of a week to take full effect. For this reason, drugs with a long half-life (e.g., amiodarone, elimination t1/2 of about 58 days) are usually started with a loading dose to achieve their desired clinical effect more quickly.
Biphasic half-life
[edit]Many drugs follow a biphasic elimination curve — first a steep slope then a shallow slope:
- STEEP (initial) part of curve —> initial distribution of the drug in the body.
- SHALLOW part of curve —> ultimate excretion of drug, which is dependent on the release of the drug from tissue compartments into the blood.
The longer half-life is called the terminal half-life and the half-life of the largest component is called the dominant half-life.[39] For a more detailed description see Pharmacokinetics § Multi-compartmental models.
See also
[edit]- Half-life, pertaining to the general mathematical concept in physics or pharmacology.
- Effective half-life
References
[edit]- ^ "Elimination Half-Life". Pharmacology in one semester. Archived from the original on 22 October 2020. Retrieved 20 February 2020.
- ^ a b "Definition of Half-Life (t1⁄2)". AIDSinfo. 19 February 2020. Archived from the original on 20 February 2020. Retrieved 20 February 2020.
- ^ Curry, Stephen H. (1993). "PHARMACOKINETICS OF ANTIPSYCHOTIC DRUGS". Antipsychotic Drugs and their Side-Effects. Elsevier. pp. 127–144. doi:10.1016/b978-0-12-079035-7.50015-4. ISBN 978-0-12-079035-7.
The elimination half-life measures the kinetics of loss of drug from the body as a whole once all distribution equilibria have been achieved.
- ^ a b Dasgupta, Amitava; Krasowski, Matthew D. (2020). "Pharmacokinetics and therapeutic drug monitoring". Therapeutic Drug Monitoring Data. Elsevier. pp. 1–17. doi:10.1016/b978-0-12-815849-4.00001-3. ISBN 978-0-12-815849-4. S2CID 209258489.
The half-life of a drug is the time required for the serum concentration to be reduced by 50%. Once the half-life of the drug is known, the time required for clearance can be estimated. Approximately 97% of the drug is eliminated by 5 halflives, while ~99% is eliminated by 7 half-lives.
- ^ Toutain, P. L.; Bousquet-Melou, A. (2004). "Plasma terminal half-life" (PDF). Journal of Veterinary Pharmacology and Therapeutics. 27 (6): 427–439. doi:10.1111/j.1365-2885.2004.00600.x. PMID 15601438. Archived from the original (PDF) on 20 February 2020.
Following i.v. administration, the terminal half-life is the time required for plasma/blood concentration to decrease by 50% after pseudo-equilibrium of distribution has been reached; then, terminal half-life is computed when the decrease in drug plasma concentration is due only to drug elimination, and the term 'elimination half-life' is applicable. Therefore, it is not the time necessary for the amount of the administered drug to fall by one half.
- ^ IUPAC, Compendium of Chemical Terminology, 2nd ed. (the "Gold Book") (1997). Online corrected version: (2006–) "Biological Half Life". doi:10.1351/goldbook.B00658
- ^ Lin VW; Cardenas DD (2003). Spinal Cord Medicine. Demos Medical Publishing, LLC. p. 251. ISBN 1-888799-61-7.
- ^ Nordberg, Gunnar (2007). Handbook on the toxicology of metals. Amsterdam: Elsevier. p. 119. ISBN 978-0-12-369413-3.
- ^ Silk, Kenneth R.; Tyrer, Peter J. (2008). Cambridge textbook of effective treatments in psychiatry. Cambridge, UK: Cambridge University Press. p. 295. ISBN 978-0-521-84228-0.
- ^ Haberfeld H, ed. (2020). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Adenosin Baxter3 mg/ml Injektionslösung.
- ^ Haberfeld H, ed. (2020). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Noradrenalin Orpha 1 mg/ml Konzentrat zur Herstellung einer Infusionslösung.
- ^ Ehrsson, Hans; et al. (Winter 2002). "Pharmacokinetics of oxaliplatin in humans". Medical Oncology. 19 (4): 261–5. doi:10.1385/MO:19:4:261. PMID 12512920. S2CID 1068099. Archived from the original on 28 September 2007. Retrieved 28 March 2007.
- ^ Zaleplon Monograph. Accessed 15 April 2021.
- ^ Morphine Monograph. Accessed 15 April 2021.
- ^ a b Flurazepam Monograph. Accessed 15 April 2021.
- ^ "Trexall, Otrexup (methotrexate) dosing, indications, interactions, adverse effects, and more". reference.medscape.com.
- ^ Manfredonia, John (March 2005). "Prescribing Methadone for Pain Management in End-of-Life Care". Journal of the American Osteopathic Association. 105 (3 supplement): S18-21. PMID 18154194. Archived from the original on 20 May 2007. Retrieved 29 January 2007.
- ^ a b Diazepam Monograph. Accessed 15 April 2021.
- ^ Haberfeld H, ed. (2020). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Epilan D 100 mg-Tabletten.
- ^ Buprenorphine Monograph. Accessed 15 April 2021.
- ^ "Klonopin (clonazepam) Prescribing Guide" (PDF). Genentech USA, Inc. October 2017. Retrieved 20 January 2019.
- ^ Asiri, Yousif A.; Mostafa, Gamal A.E. (2010). "Donepezil". Profiles of Drug Substances, Excipients and Related Methodology. Vol. 35. Elsevier. pp. 117–150. doi:10.1016/s1871-5125(10)35003-5. ISBN 978-0-12-380884-4. ISSN 1871-5125. PMID 22469221.
Plasma donepezil concentrations decline with a half-life of approximately 70 h. Sex, race, and smoking history have no clinically significant influence on plasma concentrations of donepezil [46–51].
{{cite book}}:|journal=ignored (help) - ^ a b Fluoxetine Monograph. Accessed 15 April 2021.
- ^ Haberfeld H, ed. (2020). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Sedacoron 200 mg-Tabletten.
- ^ "Caprelsa (vandetanib) Tablets, for Oral Use. Full Prescribing Information" (PDF). Sanofi Genzyme, Cambridge, MA, Dec 2016. Retrieved 24 February 2020.
- ^ Haberfeld H, ed. (2020). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Avodart 0,5 mg Weichkapseln.
- ^ "Sirturo (bedaquiline) Tablets. Full Prescribing Information" (PDF). Janssen Products, Dec 2012. Retrieved 24 February 2020.
- ^ Nikolas C Papanikolaou; Eleftheria G Hatzidaki; Stamatis Belivanis; George N Tzanakakis; Aristidis M Tsatsakis (2005). "Lead toxicity update. A brief review". Medical Science Monitor. 11 (10): RA329-36. PMID 16192916.
- ^ Griffin et al. 1975 as cited in ATSDR 2005
- ^ Rabinowitz et al. 1976 as cited in ATSDR 2005
- ^ a b Baribeau, Danielle A; Anagnostou, Evdokia (2015). "Oxytocin and vasopressin: linking pituitary neuropeptides and their receptors to social neurocircuits". Frontiers in Neuroscience. 9: 335. doi:10.3389/fnins.2015.00335. ISSN 1662-453X. PMC 4585313. PMID 26441508.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 7: Neuropeptides". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 195. ISBN 9780071481274.
Oxytocin can be delivered to humans via nasal spray following which it crosses the blood–brain barrier. ... In a double-blind experiment, oxytocin spray increased trusting behavior compared to a placebo spray in a monetary game with real money at stake.
- ^ McGregor IS, Callaghan PD, Hunt GE (May 2008). "From ultrasocial to antisocial: a role for oxytocin in the acute reinforcing effects and long-term adverse consequences of drug use?". British Journal of Pharmacology. 154 (2): 358–68. doi:10.1038/bjp.2008.132. PMC 2442436. PMID 18475254.
Recent studies also highlight remarkable anxiolytic and prosocial effects of intranasally administered OT in humans, including increased 'trust', decreased amygdala activation towards fear-inducing stimuli, improved recognition of social cues and increased gaze directed towards the eye regions of others (Kirsch et al., 2005; Kosfeld et al., 2005; Domes et al., 2006; Guastella et al., 2008)
- ^ Weisman O, Zagoory-Sharon O, Feldman R (2012). "Intranasal oxytocin administration is reflected in human saliva". Psychoneuroendocrinology. 37 (9): 1582–6. doi:10.1016/j.psyneuen.2012.02.014. PMID 22436536. S2CID 25253083.
- ^ Huffmeijer R, Alink LR, Tops M, Grewen KM, Light KC, Bakermans-Kranenburg MJ, Ijzendoorn MH (2012). "Salivary levels of oxytocin remain elevated for more than two hours after intranasal oxytocin administration". Neuro Endocrinology Letters. 33 (1): 21–5. PMID 22467107.
- ^ Miles Hacker; William S. Messer; Kenneth A. Bachmann (19 June 2009). Pharmacology: Principles and Practice. Academic Press. p. 205. ISBN 978-0-08-091922-5.
- ^ Frymoyer, Adam (2019). "Pharmacokinetic Considerations in Neonates". Infectious Disease and Pharmacology. pp. 123–139. doi:10.1016/B978-0-323-54391-0.00011-4. ISBN 9780323543910. S2CID 57512164.
- ^ Chan, Patrick; Uchizono, James A. (2015). "Pharmacokinetics and Pharmacodynamics of Anesthetics". Essentials of Pharmacology for Anesthesia, Pain Medicine, and Critical Care. pp. 3–47. doi:10.1007/978-1-4614-8948-1_1. ISBN 978-1-4614-8947-4.
- ^ a b c Bonate, Peter L.; Howard, Danny R. (2004). Clinical study design and analysis. Arlington, VA: AAPS Press. pp. 237–239. ISBN 9780971176744.
- ^ Toutain, P. L.; Bousquet-Melou, A. (2004). "Plasma terminal half-life". Journal of Veterinary Pharmacology and Therapeutics. 27 (6): 427–439. doi:10.1111/j.1365-2885.2004.00600.x. ISSN 0140-7783. PMID 15601438.
- ^ Younggil Kwon (8 May 2007). Handbook of Essential Pharmacokinetics, Pharmacodynamics and Drug Metabolism for Industrial Scientists. Springer Science & Business Media. pp. 24–. ISBN 978-0-306-46820-9.








